Bone related injuries occur in different rates in different sports. These include fractures or bone stress-related incidents. Injuries can be acute, like falling on an outstretched arm and fracturing the wrist; or they can be chronic, like stress fractures that accumulate over time due to inadequate rest or nutrition deficiencies.
Athletes are exposed to more frequent injuries of the legs in certain sports like soccer, football or rugby. Upper body injuries are more frequent in sports like baseball, volleyball or gymnastics.
Many athletes and coaches are often unsure of when to refer out for diagnostic imaging (MRI, x-ray) to rule out a serious injury like a fracture. Sometimes, an obvious injury like falling from a box onto the head, would warrant immediate referral to the ER. Other times, a deep, dull, aching discomfort that has been present for weeks may not be overly suspicious, but can still be a sign of a more serious injury to an observant individual.
Athletes may be encouraged to use ice, rest and different braces to manage pain while continuing to participate in sport. This may be a modestly effective treatment for some injuries, but it can be disastrous for others.
Sports related injuries of the neck, knee and ankle can cause a range of symptoms from mild discomfort to severe and debilitating pain. Having a health care provider onsite at the time of injury is always the best. However, in the event that one is not available, coaches, parents or athletes may need to determine how to best address the injured athlete in front of them.
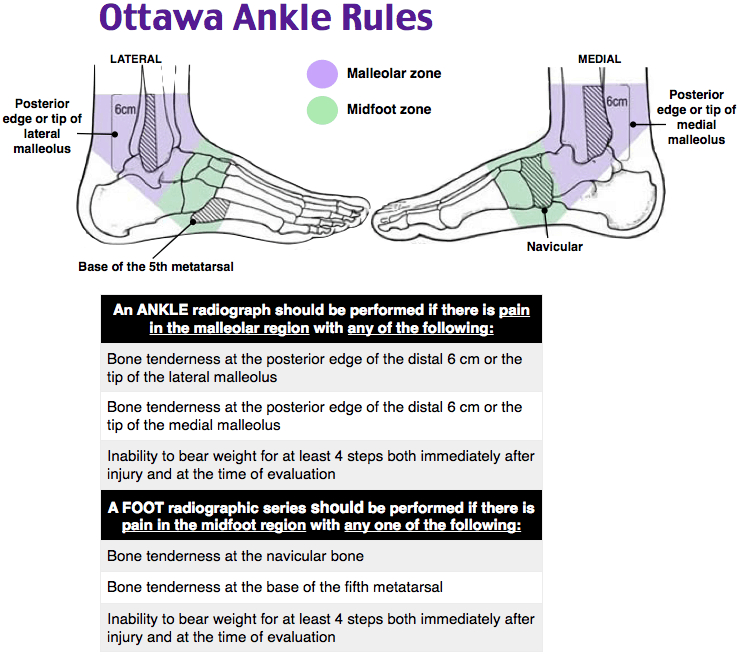
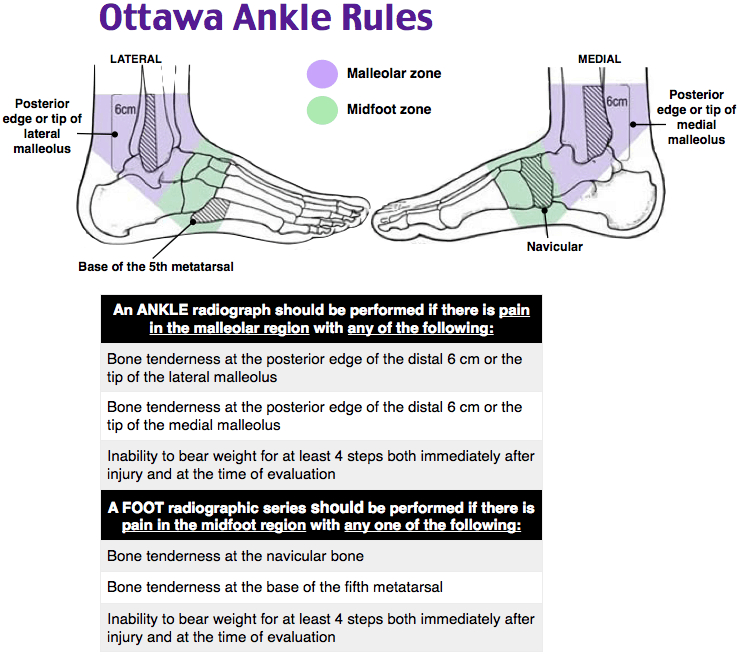
Using algorithms to determine the best imaging can help reduce health care costs, time and unnecessary exposure to radiation. The Ottawa Rules were designed to assist clinicians with determining when to refer an individual for radiographs (x-rays) when admitted to the emergency room.
The creator, Dr. Ian Stiell states “We found that emergency doctors were ordering many imaging studies for ankle injuries that were then found to be normal. I thought if there were a set a rules with criteria developed by emergency physicians, for emergency physicians, they would help this problem and shorten emergency department wait times and costs.”
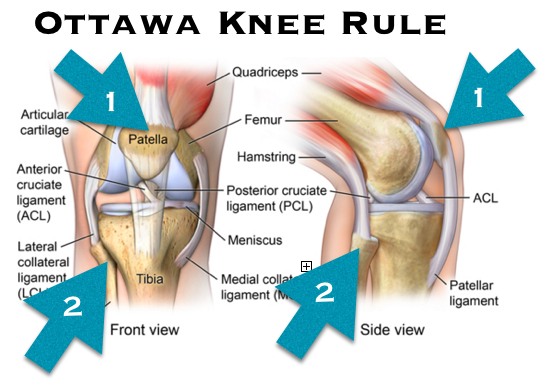
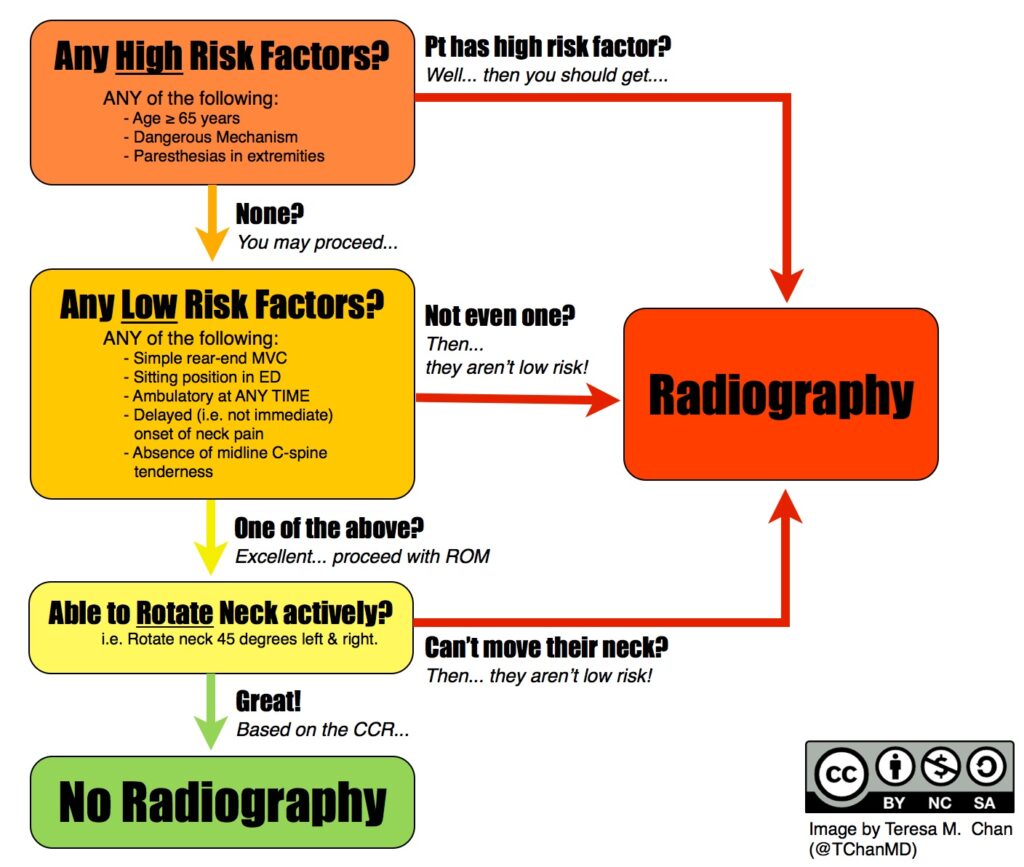
Below are the algorithms used to determine proper referral for imaging for the ankle, knee, neck and head.
Each algorithm is designed to be as sensitive as possible. That means that the researchers wanted to minimize the number of people that should have been referred for radiographs, but weren’t.
These tests should be administered by a qualified health care provider.
The Ottawa ankle rule states that if the person has tenderness on at least one of the points indicated on the picture and cannot bear weight on the injured foot for at least 5 steps, they should be referred for x-ray.
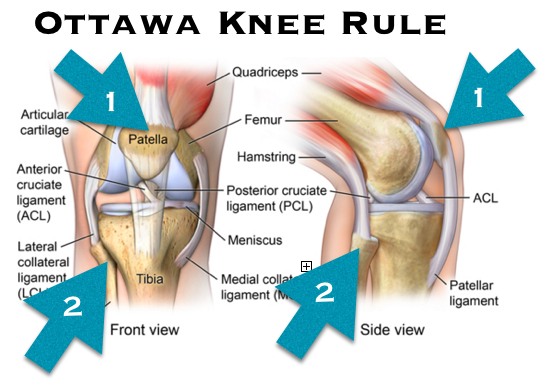
The Ottawa knee rule states that if the person is older than 55, has tenderness to the patella (knee cap) or fibular head, cannot bend the knee more than 90 degrees, and cannot walk 4 weight bearing steps, they should be referred for radiographs.
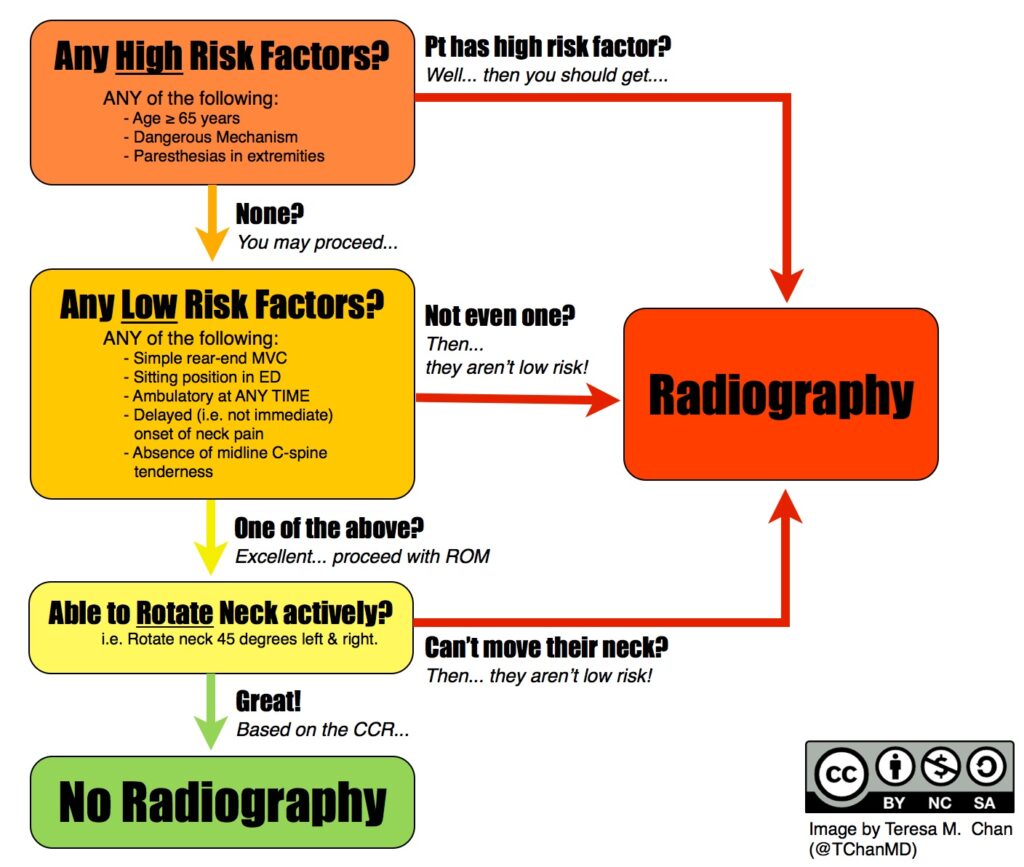
The Canadia C-Spine rules follow a flow chart, ruling out specific risk factors, directing to radiographs or additional questions, until all questions are satisfied.
The Canadian CT Head Injury requires quite a bit more medical knowledge. The assessment begins with a measurement of consciousness, then proceeds to a risk factor flow chart. The clinician then determines the utility in ordering a CT scan of the head.
The information present in this post should not substitute medical advice. Direct communication with a health care professional should always be the first option.

The information present in this post should not substitute medical advice. Direct communication with a health care professional should always be the first option.
Bone related injuries occur in different rates in different sports. These include fractures or bone stress-related incidents. Injuries can be acute, like falling on an outstretched arm and fracturing the wrist; or they can be chronic, like stress fractures that accumulate over time due to inadequate rest or nutrition deficiencies.
Athletes are exposed to more frequent injuries of the legs in certain sports like soccer, football or rugby. Upper body injuries are more frequent in sports like baseball, volleyball or gymnastics.
Many athletes and coaches are often unsure of when to refer out for diagnostic imaging (MRI, x-ray) to rule out a serious injury like a fracture. Sometimes, an obvious injury like falling from a box onto the head, would warrant immediate referral to the ER. Other times, a deep, dull, aching discomfort that has been present for weeks may not be overly suspicious, but can still be a sign of a more serious injury to an observant individual.
Athletes may be encouraged to use ice, rest and different braces to manage pain while continuing to participate in sport. This may be a modestly effective treatment for some injuries, but it can be disastrous for others.
Sports related injuries of the neck, knee and ankle can cause a range of symptoms from mild discomfort to severe and debilitating pain. Having a health care provider onsite at the time of injury is always the best. However, in the event that one is not available, coaches, parents or athletes may need to determine how to best address the injured athlete in front of them.
Using algorithms to determine the best imaging can help reduce health care costs, time and unnecessary exposure to radiation. The Ottawa Rules were designed to assist clinicians with determining when to refer an individual for radiographs (x-rays) when admitted to the emergency room.
The creator, Dr. Ian Stiell states “We found that emergency doctors were ordering many imaging studies for ankle injuries that were then found to be normal. I thought if there were a set a rules with criteria developed by emergency physicians, for emergency physicians, they would help this problem and shorten emergency department wait times and costs.”
Below are the algorithms used to determine proper referral for imaging for the ankle, knee, neck and head.
Each algorithm is designed to be as sensitive as possible. That means that the researchers wanted to minimize the number of people that should have been referred for radiographs, but weren’t.
These tests should be administered by a qualified health care provider.
The Ottawa ankle rule states that if the person has tenderness on at least one of the points indicated on the picture and cannot bear weight on the injured foot for at least 5 steps, they should be referred for x-ray.
The Ottawa knee rule states that if the person is older than 55, has tenderness to the patella (knee cap) or fibular head, cannot bend the knee more than 90 degrees, and cannot walk 4 weight bearing steps, they should be referred for radiographs.
The Canadia C-Spine rules follow a flow chart, ruling out specific risk factors, directing to radiographs or additional questions, until all questions are satisfied.
The Canadian CT Head Injury requires quite a bit more medical knowledge. The assessment begins with a measurement of consciousness, then proceeds to a risk factor flow chart. The clinician then determines the utility in ordering a CT scan of the head.
The information present in this post should not substitute medical advice. Direct communication with a health care professional should always be the first option.