Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
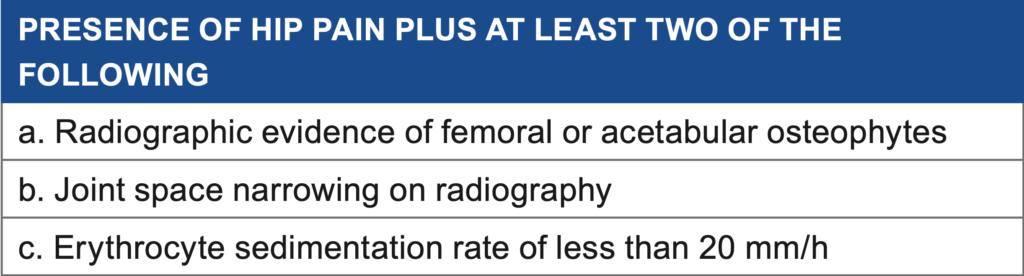
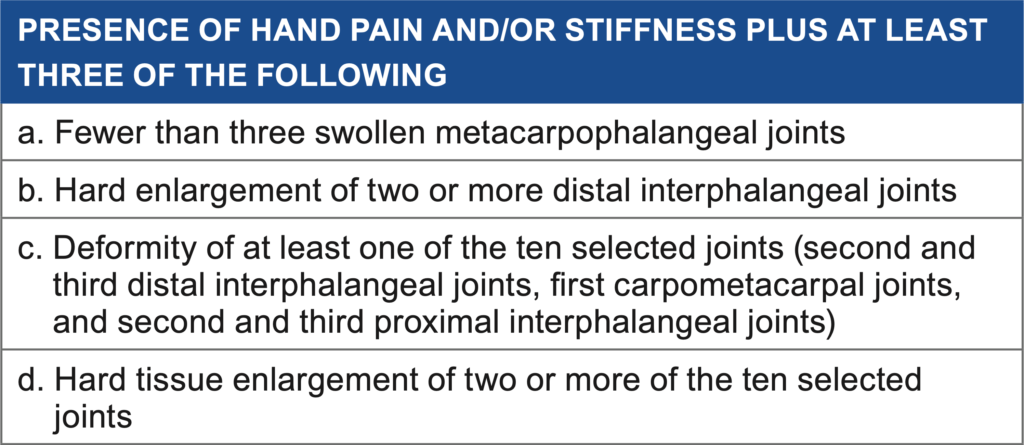
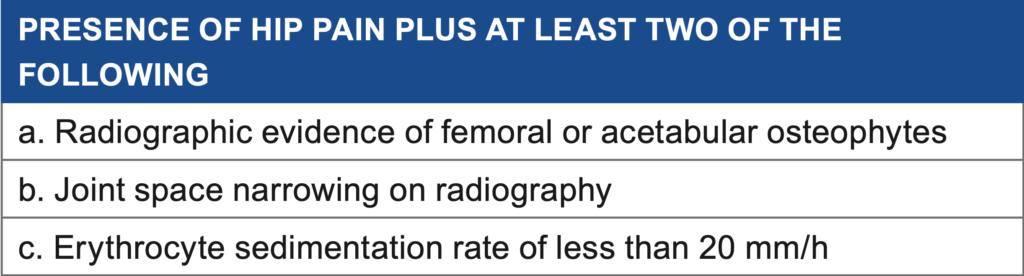
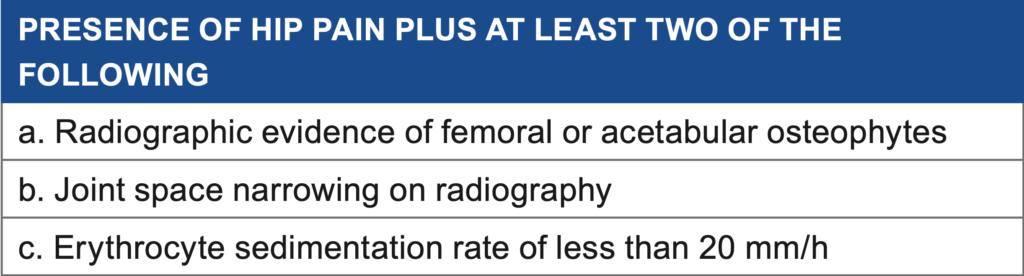
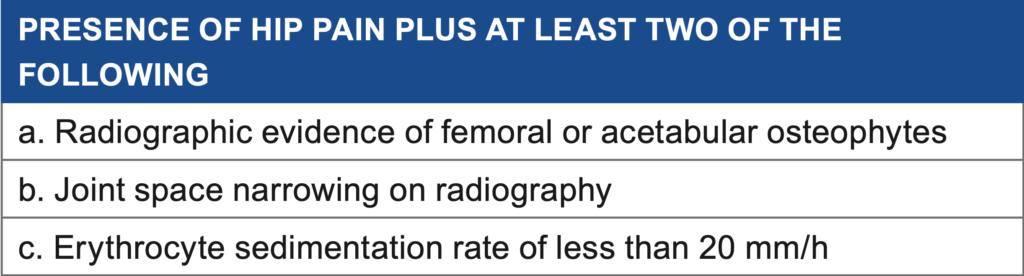
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
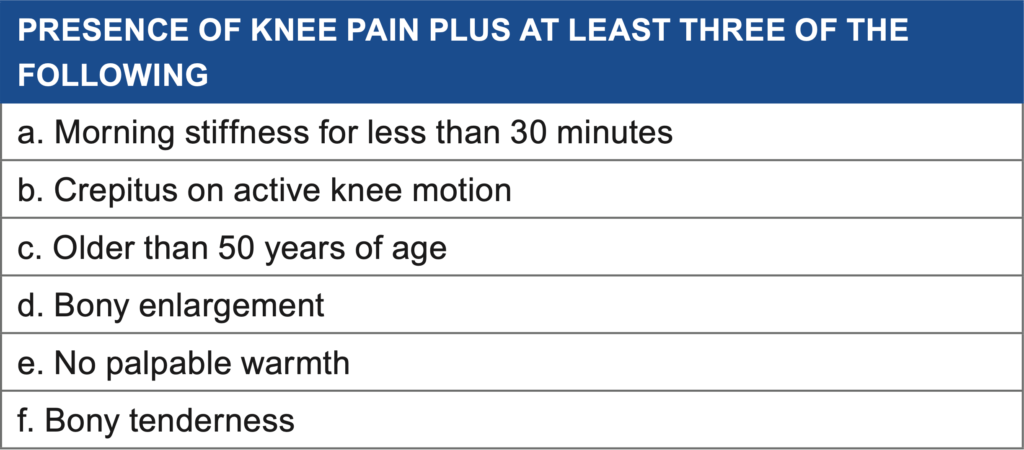
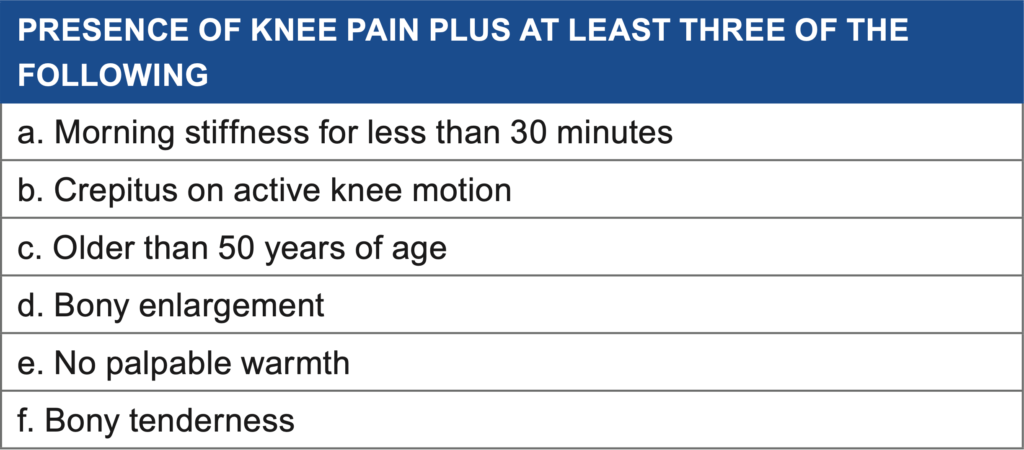
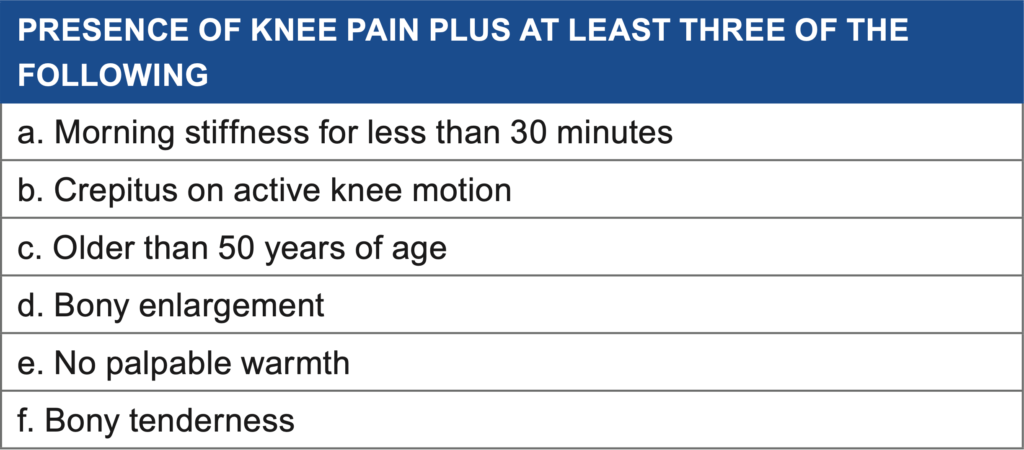
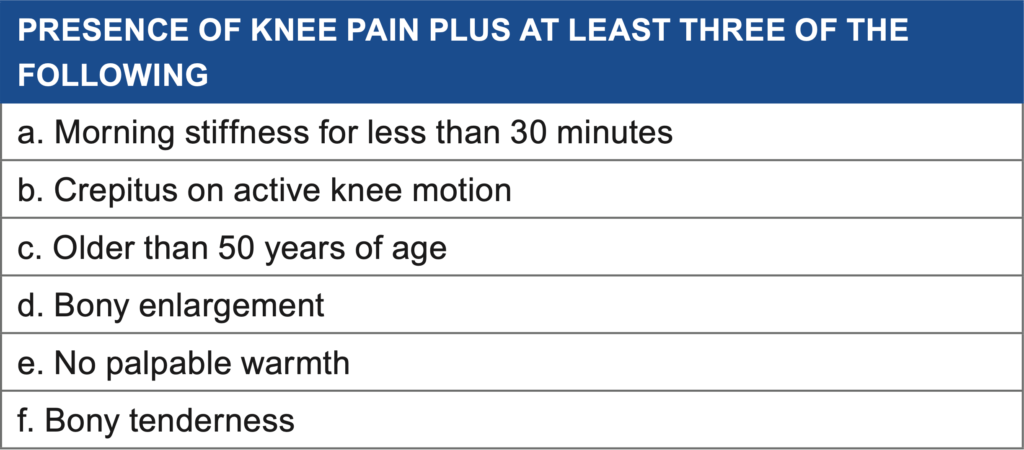
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
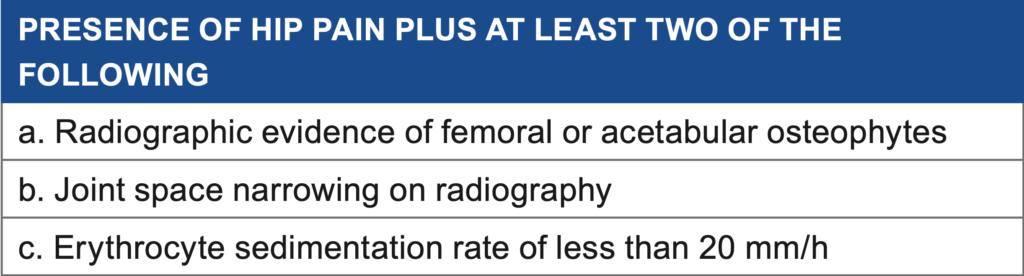
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
Sports that cause direct trauma to joints, including football, soccer, lacrosse and rugby, account for most of the traumatic onset. About 80% of former football players developed OA 10-30 years after competing. One component of the athletic endeavor includes a higher rate of loading and frequency, disrupting cartilage repair.
Cartilage is designed to withstand compressive forces. However, if inadequate time is allowed for the tissue to rest, the surface may become damaged, exposing sensitive tissue underneath.
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
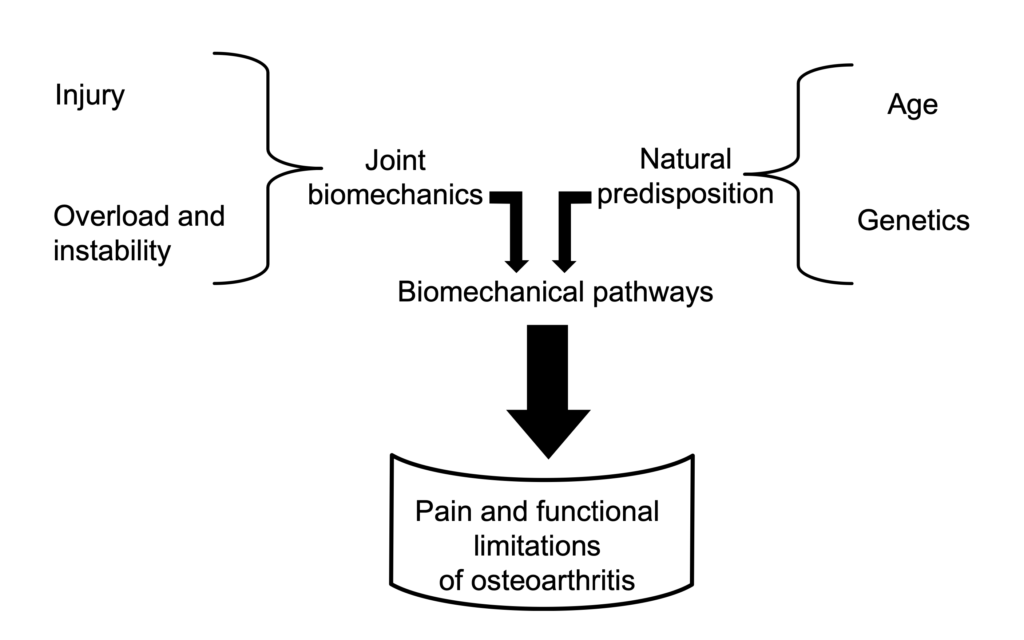
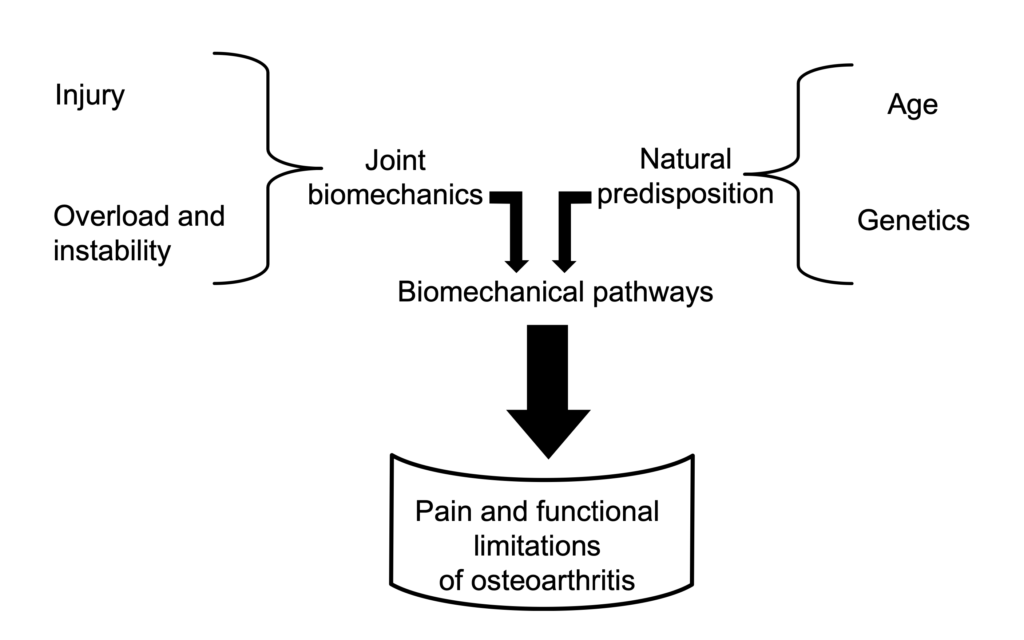
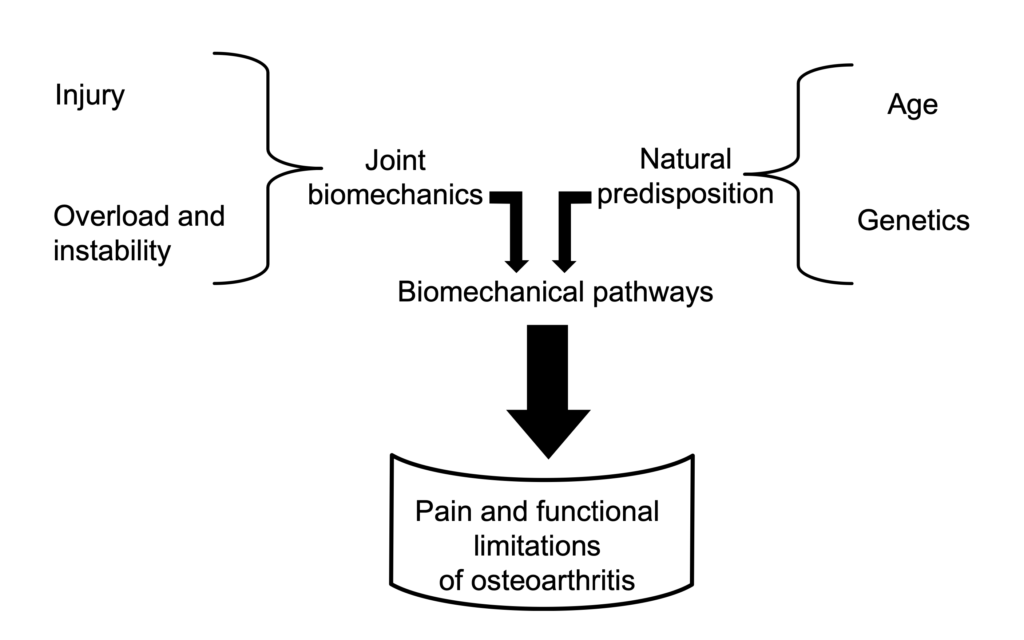
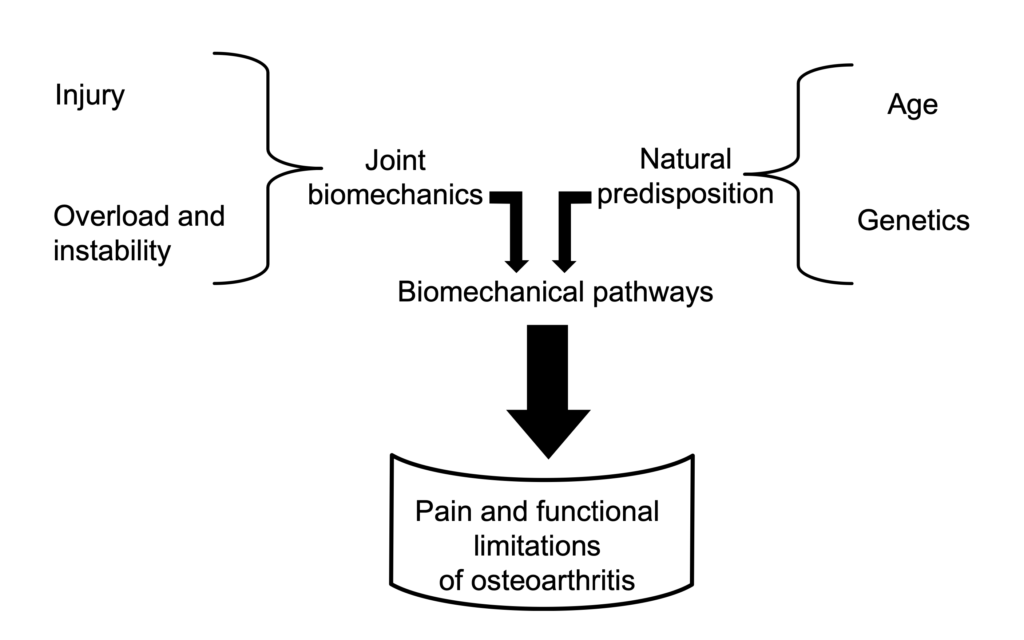
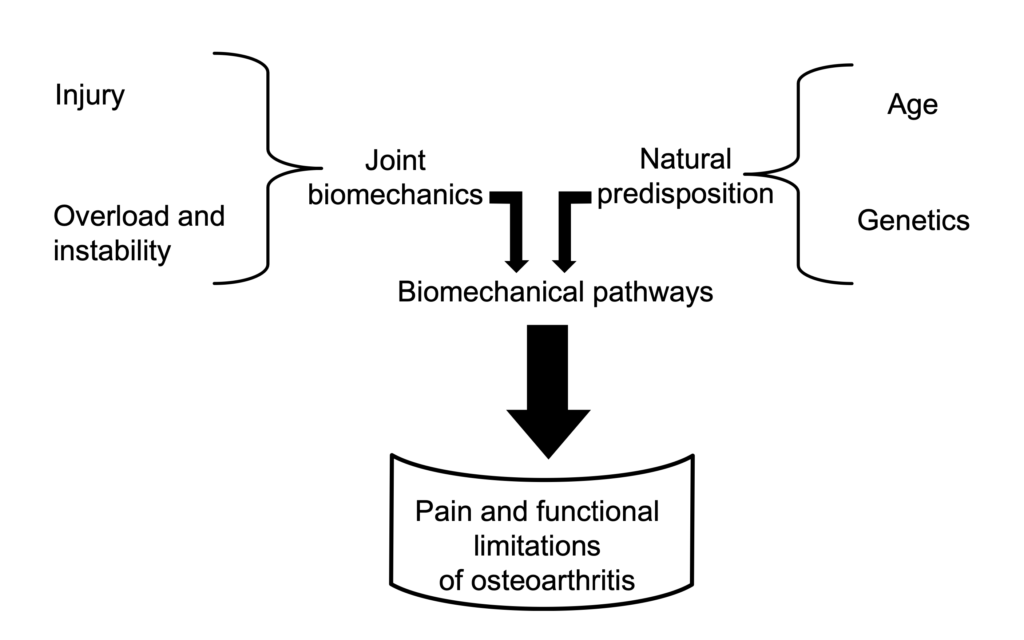
Genetics, obesity, joint injury, occupation, gender and race are risk factors for the onset and progression of OA.
Sports that cause direct trauma to joints, including football, soccer, lacrosse and rugby, account for most of the traumatic onset. About 80% of former football players developed OA 10-30 years after competing. One component of the athletic endeavor includes a higher rate of loading and frequency, disrupting cartilage repair.
Cartilage is designed to withstand compressive forces. However, if inadequate time is allowed for the tissue to rest, the surface may become damaged, exposing sensitive tissue underneath.
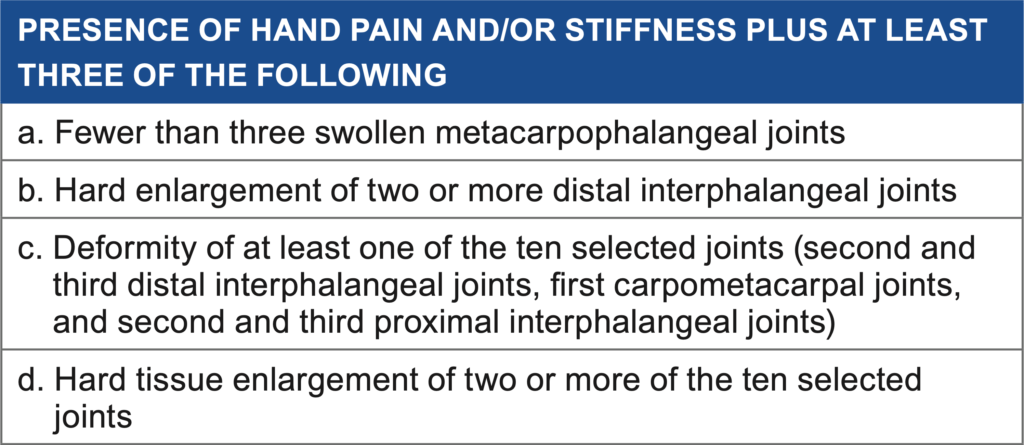
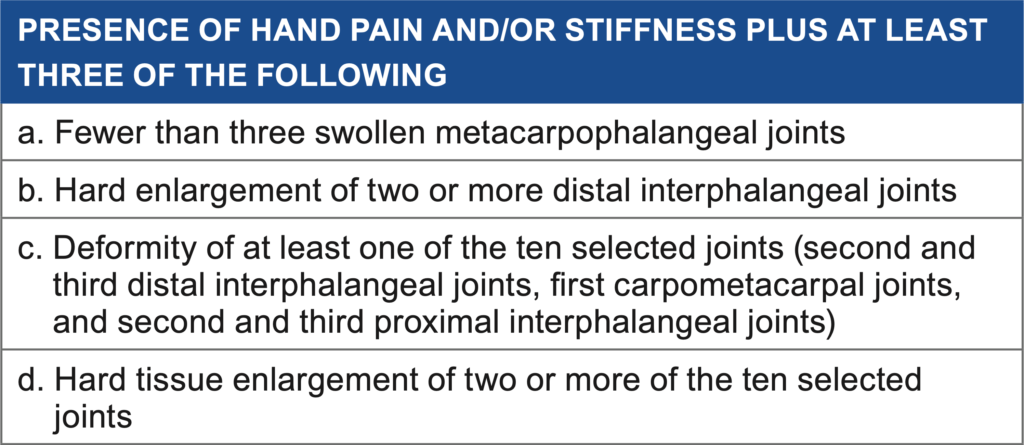
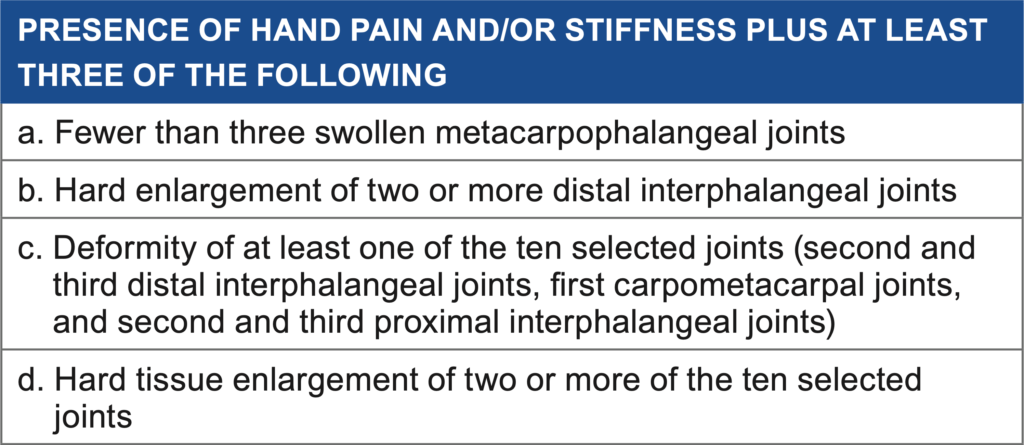
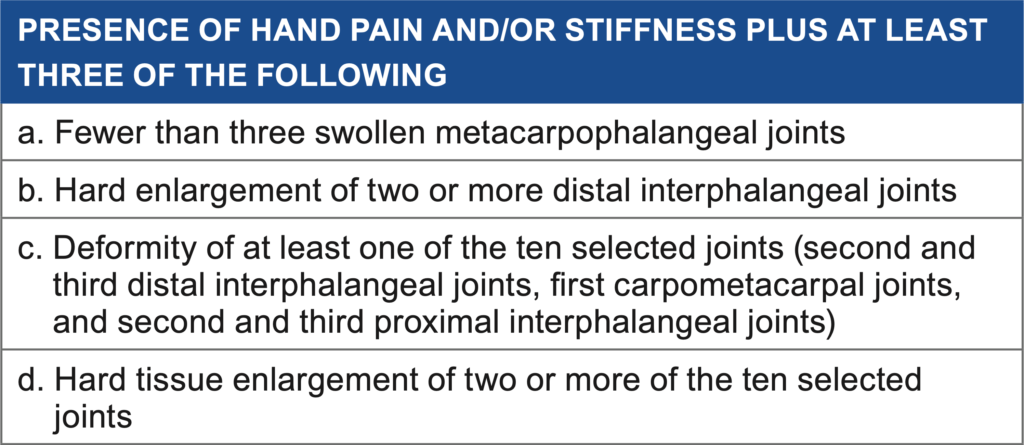
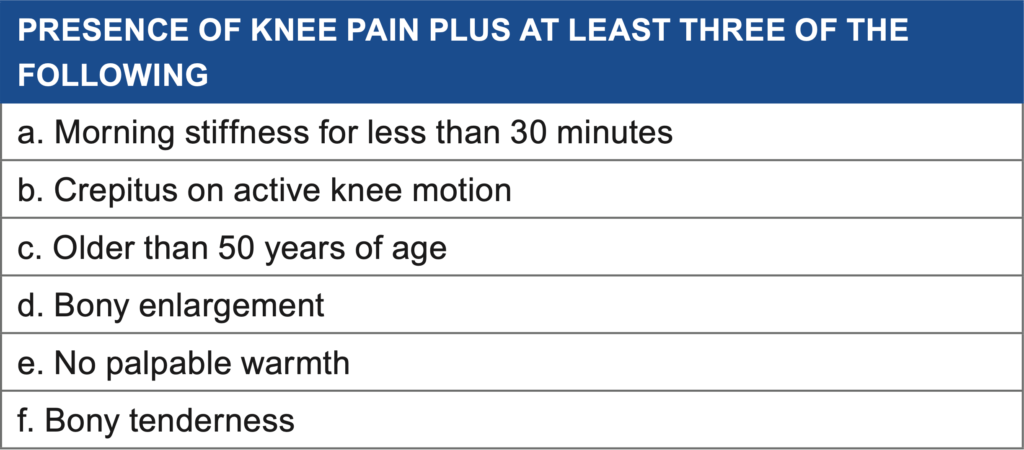
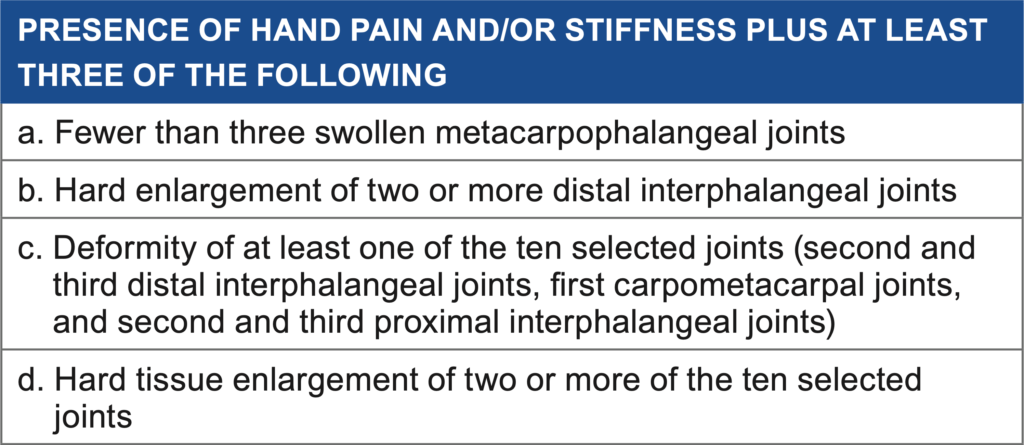
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
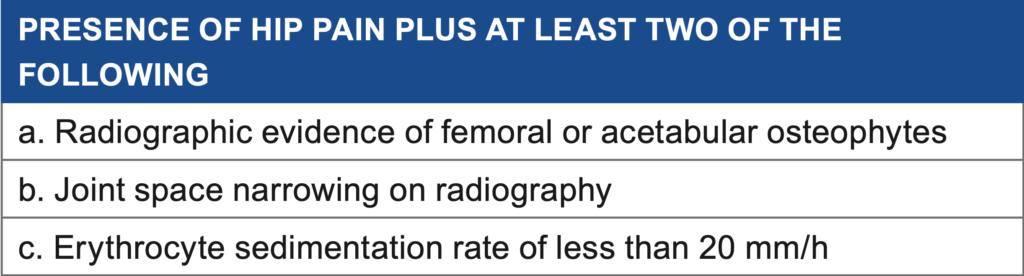
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.

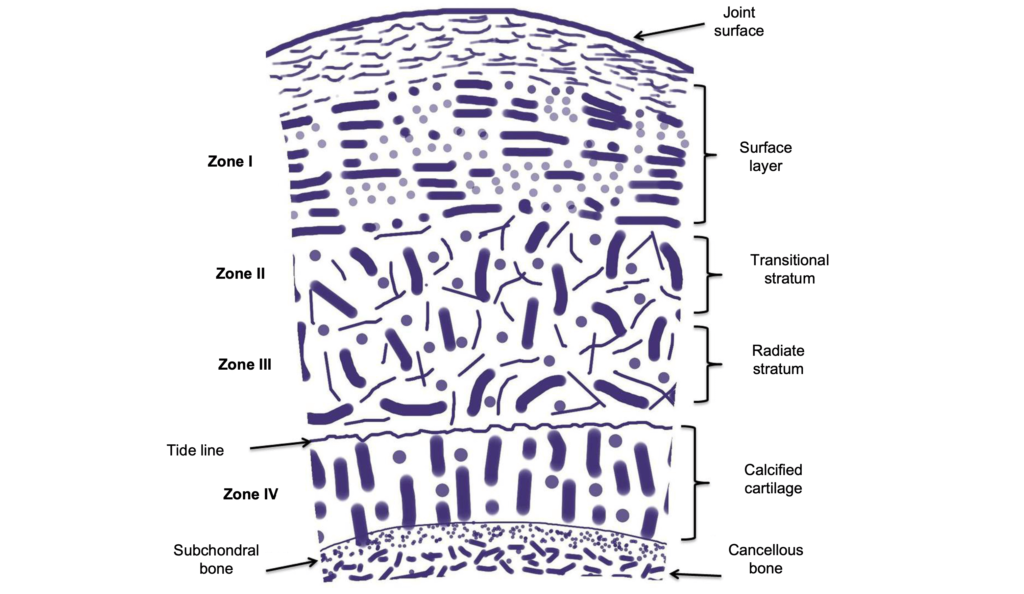
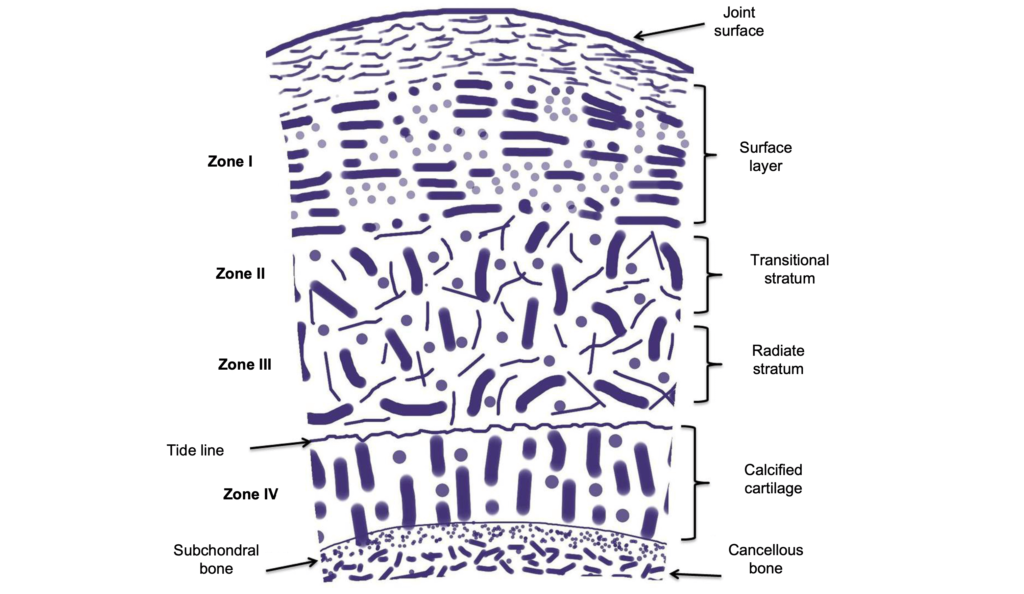
Osteoarthritis (OA) is caused by a defect in the joint cartilage. Cartilage is a soft, spongy type of tissue, well lubricated, designed to minimize friction between two surfaces. As we age, the cartilage becomes less lubricated, wearing out the more superficial layers, resulting in pain & dysfunction.
Genetics, obesity, joint injury, occupation, gender and race are risk factors for the onset and progression of OA.
Sports that cause direct trauma to joints, including football, soccer, lacrosse and rugby, account for most of the traumatic onset. About 80% of former football players developed OA 10-30 years after competing. One component of the athletic endeavor includes a higher rate of loading and frequency, disrupting cartilage repair.
Cartilage is designed to withstand compressive forces. However, if inadequate time is allowed for the tissue to rest, the surface may become damaged, exposing sensitive tissue underneath.
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.