You will not find another physical therapist in all of Miami that has helped out high caliber athletes like me. I guarantee that.
The second is improved pain tolerance. Pain tolerance is the maximal intensity of pain someone is willing to tolerate. For example, how long can that person maximally squeeze your fingers before you tell them to stop?
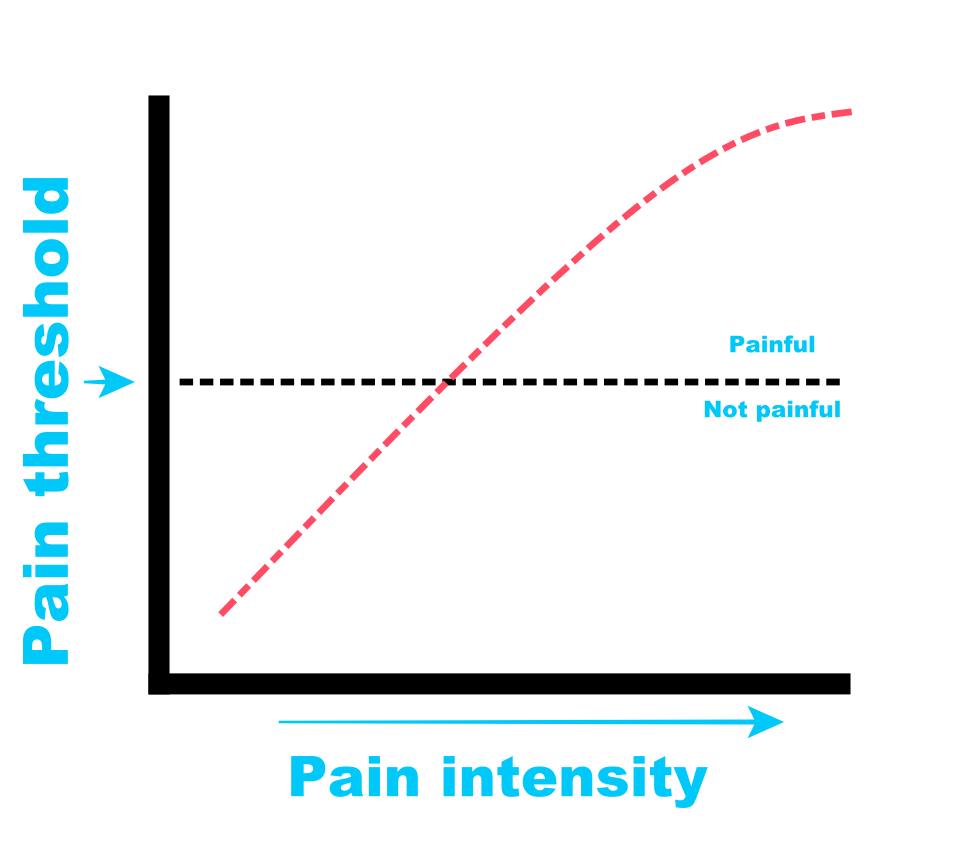
Exercise can improve pain threshold and pain tolerance.
Exercise can also improve pain perception at the neurological level.
A third benefit is temporal summation, or the increase in pain after repetitive stimulation at the same intensity, can be reduced. For example, if every time you raised your hand overhead, how many times could you do it before it becomes unbearable? Exercise-induced pain relief can increase the number of “reps”, so to speak, that can be performed before reaching the pain tolerance.
A fourth benefit of exercise to manage pain is conditioned pain modulation. This is a measurement of strength of pain inhibition. Pain modulation allows for progressively painful stimuli to be perceived as non-threatening.
A fifth benefit is improving how the brain processes pain. When exposed to pain, the brain responds by adjusting its attention through various chemicals and neurological signals. Exercise can make this response more profound by minimizing the “excitement” around the pain experience.
To summarize: improved pain threshold, improved pain tolerance, movement becomes more manageable, better pain-response conditioning and improved pain processing.
So now you might be asking:
Any and all of it really. Studies over the past 2 decades show consistent improvements in the pain experience regardless of the type of exercise and the duration. However, there is a intensity-dose curve. The more intense and painful (not injury/pathological pain) the exercise is, the better the pain management.
The neat thing about the “openness” of choosing your preferred mode of exercise, is that even the non-exercised body part can experience reductions in pain. For example, if you have shoulder pain and you want to avoid a repeat injury from doing an upper body workout, simply get on a bike or treadmill and work the lower body. How cool is that?
Studies demonstrate a 15-20% reduction in pain of the injured body part even when exercising non-injured limbs!
Choose your exercise medicine! You can bike, swim, or run. You can do traditional strength training, isometric training or plyometric training. You can workout by yourself, or you can join a group fitness class.
It doesn’t really matter when it comes to exercise selection and pain relief.
What does matter is the exercise intensity and duration.
To summarize: Studies exposing people to higher intensity and longer duration exercises seem to have much better tolerance and thresholds.
For one, treatment expectations can have a profound impact. Individuals who have a positive outlook and favorable view of exercise tend to experience greater benefits.
If the person perceives exercise as non-threatening, they tend to do better. People that perceive exercise to potentially make their condition worse, tend to do worse.
Very often doctors and friends will discuss the condition and make it sound scary or threatening. This happens very often with knee arthritis and x-rays. The x-ray will show “bone on bone” and the doctor will explain that this is the cause of pain. They may also throw in that continuing to exercise, or run or bike or whatever will make the condition worse.
Categorically not true! And that is such a beautiful thing! Research has consistently demonstrated that there is absolutely no correlation between pain levels and diagnostic imaging. People can have x-rays showing the worst kinds of findings have no pain at all and continue to go about their lives playing sports and going out to socialize.
Hearing from a medical authority, someone you trust, that your “bone on bone” knee will be made worse with exercise can create a downward spiral of fear of activity, leading to a reduction in exercise, resulting in serious deconditioning, possibly causing even more pain in the long run.
We need to break people out of this cycle. More encouragement from health care providers on importance of regular physical activity, and better information on how resilient our human body is should be the cornerstone of the health model. Sadly, it’s not.
Secondly, physical fit people experience more robust pain relief from exercise. This includes better pain thresholds and better pain tolerance. Regular exposure to physical activity shows consistent results. In fact, regular exercise 2-3 days per week reduces the risk of low back pain by 33%. This is true even of people who have a high risk of developing chronic pain.
To summarize: personal beliefs regarding pain due to exercise can emphasize the direction of helpfulness (belief that pain during exercise will make the condition worse, may have less pain relief from exercise than someone who believes pain during exercise will improve pain).
There are several mechanisms believed to facilitate an improved pain experience. One system is the opioid and cannabinoid systems. Indeed, many pharmaceutical medications are designed to influence these two systems.
It has been shown that contracting muscles activate the opioid and cannabinoid pathways in the brain and spinal cord. These systems have receptors throughout the body that produce analgesia (pain relief) when stimulate (as in the case of exercise).
Exercise releases stress hormones in the body. These stress hormones (like growth hormone) may play a role in mediating pain. At the current writing of this article, more studies are needed to clearly define exactly how stress hormones may contribute to pain management.
Changes in pain perception, specifically the discomfort caused during exercise, may occur. Cognitive and psychosocial factors may help facilitate better self-efficacy, coping strategies, fear of pain and stress.
To summarize: receptors throughout the body, hormones and psychological disposition can influence the magnitude of exercise-induced pain relief.
tinue to exercise at an intensity, type and duration that is beneficial to you and your specific injury. Getting advice from a health care provider that is well-versed in exercise selection, prescription and support can have a profound impact on your health and well-being.
If you are in Miami, Florida and are experiencing shoulder pain, back pain or hip pain, and are unsure of how to begin the process of recovering from an injury, give our office a call. We have a tested and proven method that works with Olympic athletes to weekend warriors.
Here are a few things we discuss and help you manage with injuries:
You will not find another physical therapist in all of Miami that has helped out high caliber athletes like me. I guarantee that.
Regular exercise has profound impacts on physical and mental health. This includes cardiovascular health, stress, mood and sleep. I know for a fact that athletes ordered to “rest” to “recover” from an injury for almost any length of time, become frustrated and let down because they can’t participate in the sport they love. Sports physical therapists like myself can create mutual goals and boundaries for athletes to continue to train despite an injury offers that athlete hope and something to work towards- return to sport.
There are several benefits to continue training even when experiencing pain. These include pain threshold, pain tolerance, perception of pain and function.
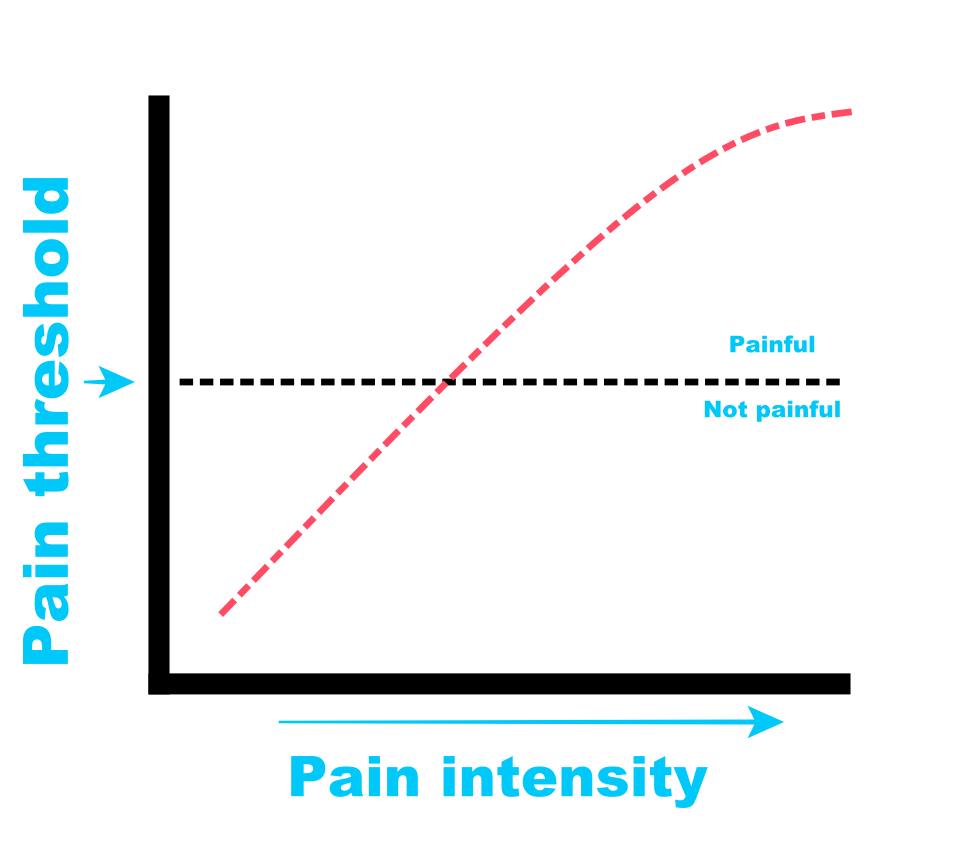
The first is improved pain threshold. The pain threshold is the minimum level of stimulus intensity that is perceived as pain. For example, if someone were to squeeze your fingers, at what point would that become painful? Exercise raises this threshold of when the pain begins.
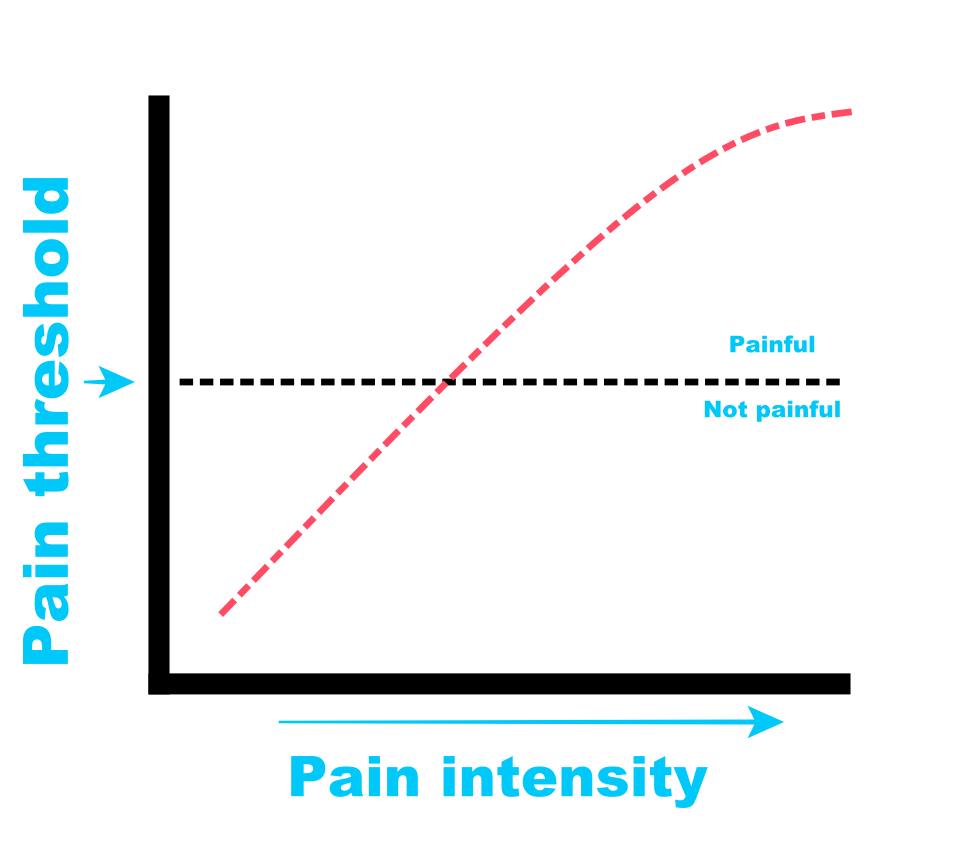
The second is improved pain tolerance. Pain tolerance is the maximal intensity of pain someone is willing to tolerate. For example, how long can that person maximally squeeze your fingers before you tell them to stop?
Exercise can improve pain threshold and pain tolerance.
Exercise can also improve pain perception at the neurological level.
A third benefit is temporal summation, or the increase in pain after repetitive stimulation at the same intensity, can be reduced. For example, if every time you raised your hand overhead, how many times could you do it before it becomes unbearable? Exercise-induced pain relief can increase the number of “reps”, so to speak, that can be performed before reaching the pain tolerance.
A fourth benefit of exercise to manage pain is conditioned pain modulation. This is a measurement of strength of pain inhibition. Pain modulation allows for progressively painful stimuli to be perceived as non-threatening.
A fifth benefit is improving how the brain processes pain. When exposed to pain, the brain responds by adjusting its attention through various chemicals and neurological signals. Exercise can make this response more profound by minimizing the “excitement” around the pain experience.
To summarize: improved pain threshold, improved pain tolerance, movement becomes more manageable, better pain-response conditioning and improved pain processing.
So now you might be asking:
Any and all of it really. Studies over the past 2 decades show consistent improvements in the pain experience regardless of the type of exercise and the duration. However, there is a intensity-dose curve. The more intense and painful (not injury/pathological pain) the exercise is, the better the pain management.
The neat thing about the “openness” of choosing your preferred mode of exercise, is that even the non-exercised body part can experience reductions in pain. For example, if you have shoulder pain and you want to avoid a repeat injury from doing an upper body workout, simply get on a bike or treadmill and work the lower body. How cool is that?
Studies demonstrate a 15-20% reduction in pain of the injured body part even when exercising non-injured limbs!
Choose your exercise medicine! You can bike, swim, or run. You can do traditional strength training, isometric training or plyometric training. You can workout by yourself, or you can join a group fitness class.
It doesn’t really matter when it comes to exercise selection and pain relief.
What does matter is the exercise intensity and duration.
To summarize: Studies exposing people to higher intensity and longer duration exercises seem to have much better tolerance and thresholds.
For one, treatment expectations can have a profound impact. Individuals who have a positive outlook and favorable view of exercise tend to experience greater benefits.
If the person perceives exercise as non-threatening, they tend to do better. People that perceive exercise to potentially make their condition worse, tend to do worse.
Very often doctors and friends will discuss the condition and make it sound scary or threatening. This happens very often with knee arthritis and x-rays. The x-ray will show “bone on bone” and the doctor will explain that this is the cause of pain. They may also throw in that continuing to exercise, or run or bike or whatever will make the condition worse.
Categorically not true! And that is such a beautiful thing! Research has consistently demonstrated that there is absolutely no correlation between pain levels and diagnostic imaging. People can have x-rays showing the worst kinds of findings have no pain at all and continue to go about their lives playing sports and going out to socialize.
Hearing from a medical authority, someone you trust, that your “bone on bone” knee will be made worse with exercise can create a downward spiral of fear of activity, leading to a reduction in exercise, resulting in serious deconditioning, possibly causing even more pain in the long run.
We need to break people out of this cycle. More encouragement from health care providers on importance of regular physical activity, and better information on how resilient our human body is should be the cornerstone of the health model. Sadly, it’s not.
Secondly, physical fit people experience more robust pain relief from exercise. This includes better pain thresholds and better pain tolerance. Regular exposure to physical activity shows consistent results. In fact, regular exercise 2-3 days per week reduces the risk of low back pain by 33%. This is true even of people who have a high risk of developing chronic pain.
To summarize: personal beliefs regarding pain due to exercise can emphasize the direction of helpfulness (belief that pain during exercise will make the condition worse, may have less pain relief from exercise than someone who believes pain during exercise will improve pain).
There are several mechanisms believed to facilitate an improved pain experience. One system is the opioid and cannabinoid systems. Indeed, many pharmaceutical medications are designed to influence these two systems.
It has been shown that contracting muscles activate the opioid and cannabinoid pathways in the brain and spinal cord. These systems have receptors throughout the body that produce analgesia (pain relief) when stimulate (as in the case of exercise).
Exercise releases stress hormones in the body. These stress hormones (like growth hormone) may play a role in mediating pain. At the current writing of this article, more studies are needed to clearly define exactly how stress hormones may contribute to pain management.
Changes in pain perception, specifically the discomfort caused during exercise, may occur. Cognitive and psychosocial factors may help facilitate better self-efficacy, coping strategies, fear of pain and stress.
To summarize: receptors throughout the body, hormones and psychological disposition can influence the magnitude of exercise-induced pain relief.
tinue to exercise at an intensity, type and duration that is beneficial to you and your specific injury. Getting advice from a health care provider that is well-versed in exercise selection, prescription and support can have a profound impact on your health and well-being.
If you are in Miami, Florida and are experiencing shoulder pain, back pain or hip pain, and are unsure of how to begin the process of recovering from an injury, give our office a call. We have a tested and proven method that works with Olympic athletes to weekend warriors.
Here are a few things we discuss and help you manage with injuries:
You will not find another physical therapist in all of Miami that has helped out high caliber athletes like me. I guarantee that.

Should you stop training if you’re injured?
No.
In this article we will discuss how strength training can improve pain and function when you are managing your injury.
The absolute WORST advice I hear from my patients on behalf of their medical doctors is to take time off and rest. Why is this the worst advice? Because it completely misses out on the benefits of regular, consistent exercise.
Even in elite athletes, deconditioning occurs quickly and can make the rehab process even longer. I’m not suggesting your continue to use the injured body part without consideration of movements or activities that make the condition worse. What I almost always encourage my patients to do is to continue with strength training and drilling techniques with modifications.
These modifications include avoiding painful movements/positions, limiting the full range of the joint to avoid pain and carefully choosing partners that can work around the injury.
Regular exercise has profound impacts on physical and mental health. This includes cardiovascular health, stress, mood and sleep. I know for a fact that athletes ordered to “rest” to “recover” from an injury for almost any length of time, become frustrated and let down because they can’t participate in the sport they love. Sports physical therapists like myself can create mutual goals and boundaries for athletes to continue to train despite an injury offers that athlete hope and something to work towards- return to sport.
There are several benefits to continue training even when experiencing pain. These include pain threshold, pain tolerance, perception of pain and function.
The first is improved pain threshold. The pain threshold is the minimum level of stimulus intensity that is perceived as pain. For example, if someone were to squeeze your fingers, at what point would that become painful? Exercise raises this threshold of when the pain begins.
The second is improved pain tolerance. Pain tolerance is the maximal intensity of pain someone is willing to tolerate. For example, how long can that person maximally squeeze your fingers before you tell them to stop?
Exercise can improve pain threshold and pain tolerance.
Exercise can also improve pain perception at the neurological level.
A third benefit is temporal summation, or the increase in pain after repetitive stimulation at the same intensity, can be reduced. For example, if every time you raised your hand overhead, how many times could you do it before it becomes unbearable? Exercise-induced pain relief can increase the number of “reps”, so to speak, that can be performed before reaching the pain tolerance.
A fourth benefit of exercise to manage pain is conditioned pain modulation. This is a measurement of strength of pain inhibition. Pain modulation allows for progressively painful stimuli to be perceived as non-threatening.
A fifth benefit is improving how the brain processes pain. When exposed to pain, the brain responds by adjusting its attention through various chemicals and neurological signals. Exercise can make this response more profound by minimizing the “excitement” around the pain experience.
To summarize: improved pain threshold, improved pain tolerance, movement becomes more manageable, better pain-response conditioning and improved pain processing.
So now you might be asking:
Any and all of it really. Studies over the past 2 decades show consistent improvements in the pain experience regardless of the type of exercise and the duration. However, there is a intensity-dose curve. The more intense and painful (not injury/pathological pain) the exercise is, the better the pain management.
The neat thing about the “openness” of choosing your preferred mode of exercise, is that even the non-exercised body part can experience reductions in pain. For example, if you have shoulder pain and you want to avoid a repeat injury from doing an upper body workout, simply get on a bike or treadmill and work the lower body. How cool is that?
Studies demonstrate a 15-20% reduction in pain of the injured body part even when exercising non-injured limbs!
Choose your exercise medicine! You can bike, swim, or run. You can do traditional strength training, isometric training or plyometric training. You can workout by yourself, or you can join a group fitness class.
It doesn’t really matter when it comes to exercise selection and pain relief.
What does matter is the exercise intensity and duration.
To summarize: Studies exposing people to higher intensity and longer duration exercises seem to have much better tolerance and thresholds.
For one, treatment expectations can have a profound impact. Individuals who have a positive outlook and favorable view of exercise tend to experience greater benefits.
If the person perceives exercise as non-threatening, they tend to do better. People that perceive exercise to potentially make their condition worse, tend to do worse.
Very often doctors and friends will discuss the condition and make it sound scary or threatening. This happens very often with knee arthritis and x-rays. The x-ray will show “bone on bone” and the doctor will explain that this is the cause of pain. They may also throw in that continuing to exercise, or run or bike or whatever will make the condition worse.
Categorically not true! And that is such a beautiful thing! Research has consistently demonstrated that there is absolutely no correlation between pain levels and diagnostic imaging. People can have x-rays showing the worst kinds of findings have no pain at all and continue to go about their lives playing sports and going out to socialize.
Hearing from a medical authority, someone you trust, that your “bone on bone” knee will be made worse with exercise can create a downward spiral of fear of activity, leading to a reduction in exercise, resulting in serious deconditioning, possibly causing even more pain in the long run.
We need to break people out of this cycle. More encouragement from health care providers on importance of regular physical activity, and better information on how resilient our human body is should be the cornerstone of the health model. Sadly, it’s not.
Secondly, physical fit people experience more robust pain relief from exercise. This includes better pain thresholds and better pain tolerance. Regular exposure to physical activity shows consistent results. In fact, regular exercise 2-3 days per week reduces the risk of low back pain by 33%. This is true even of people who have a high risk of developing chronic pain.
To summarize: personal beliefs regarding pain due to exercise can emphasize the direction of helpfulness (belief that pain during exercise will make the condition worse, may have less pain relief from exercise than someone who believes pain during exercise will improve pain).
There are several mechanisms believed to facilitate an improved pain experience. One system is the opioid and cannabinoid systems. Indeed, many pharmaceutical medications are designed to influence these two systems.
It has been shown that contracting muscles activate the opioid and cannabinoid pathways in the brain and spinal cord. These systems have receptors throughout the body that produce analgesia (pain relief) when stimulate (as in the case of exercise).
Exercise releases stress hormones in the body. These stress hormones (like growth hormone) may play a role in mediating pain. At the current writing of this article, more studies are needed to clearly define exactly how stress hormones may contribute to pain management.
Changes in pain perception, specifically the discomfort caused during exercise, may occur. Cognitive and psychosocial factors may help facilitate better self-efficacy, coping strategies, fear of pain and stress.
To summarize: receptors throughout the body, hormones and psychological disposition can influence the magnitude of exercise-induced pain relief.
tinue to exercise at an intensity, type and duration that is beneficial to you and your specific injury. Getting advice from a health care provider that is well-versed in exercise selection, prescription and support can have a profound impact on your health and well-being.
If you are in Miami, Florida and are experiencing shoulder pain, back pain or hip pain, and are unsure of how to begin the process of recovering from an injury, give our office a call. We have a tested and proven method that works with Olympic athletes to weekend warriors.
Here are a few things we discuss and help you manage with injuries:
You will not find another physical therapist in all of Miami that has helped out high caliber athletes like me. I guarantee that.