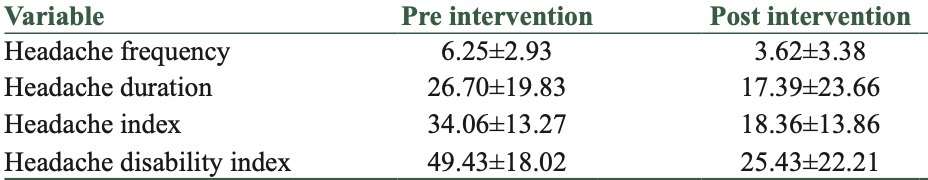
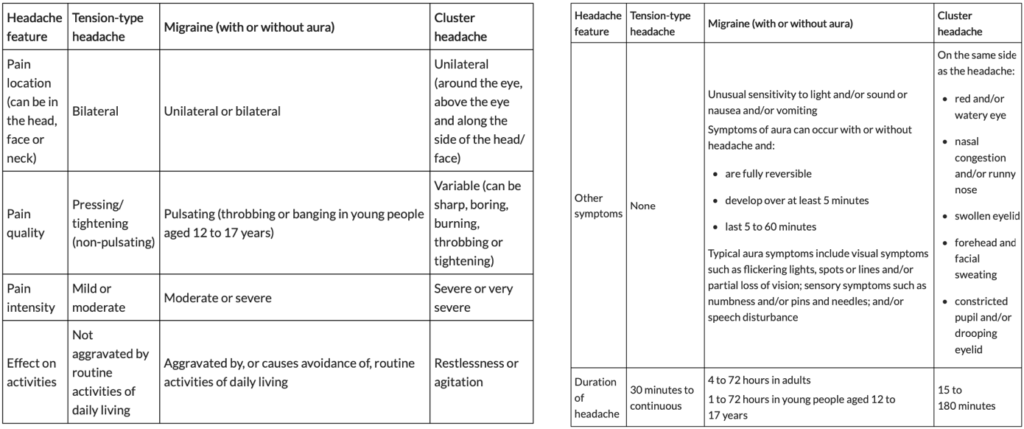
Headache features
The below chart describes headache features and commonly associated, patient-reported experiences. These include tension-type headaches, migraine and cluster headaches. Very often, these symptoms overlap, or may have distinctive features.
Tension-type headaches are often described as painful pressure/tightness. Migraines are often associated with an aura and sensitivity to light or sound. Cluster headaches may be associated with a change in vision, nasal congestion or excessive facial sweating.
Headaches can be treated with pharmacological and non-pharmacological interventions.
Pharmacological interventions include medication. Non-pharmacological intervention can include physical therapy and cognitive-behavioral therapy.
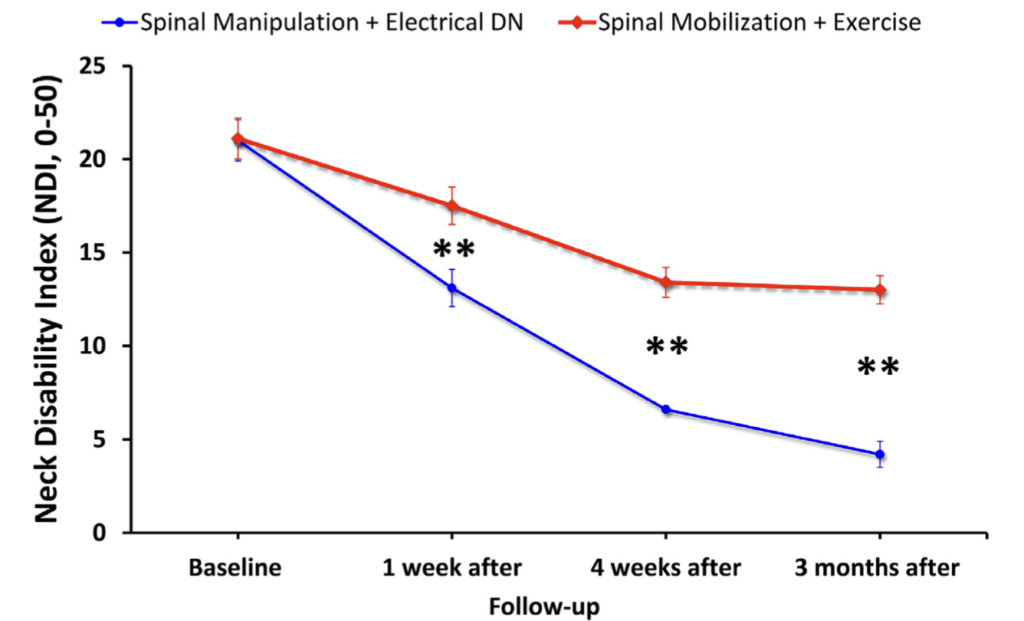
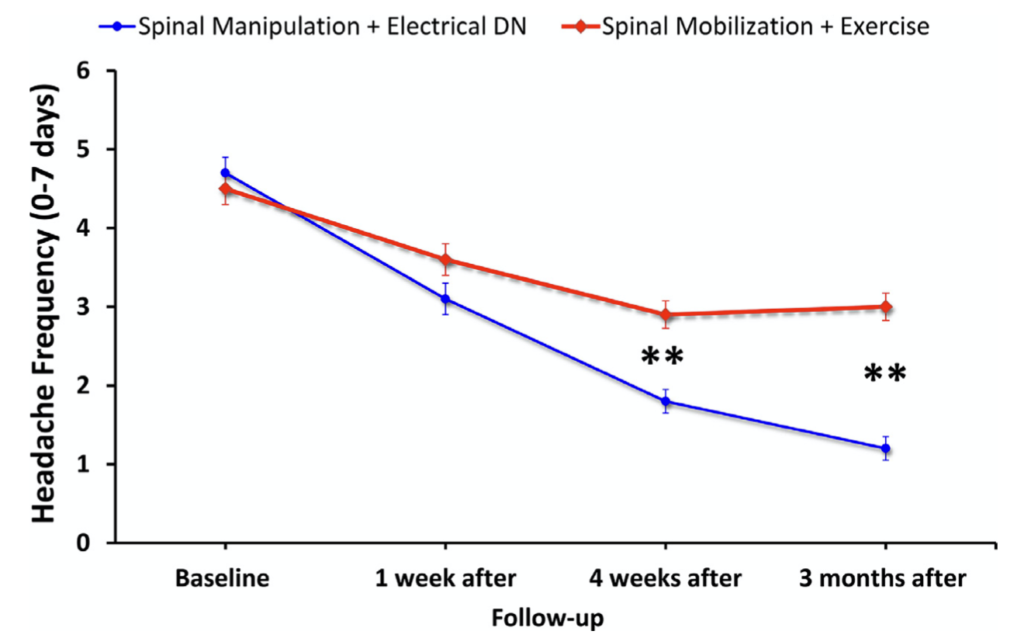
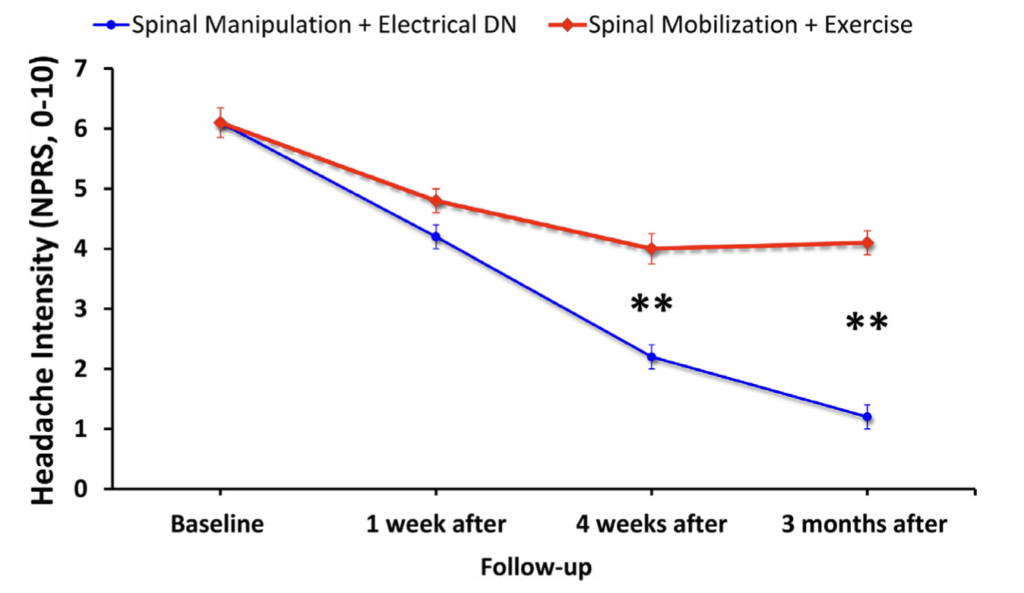
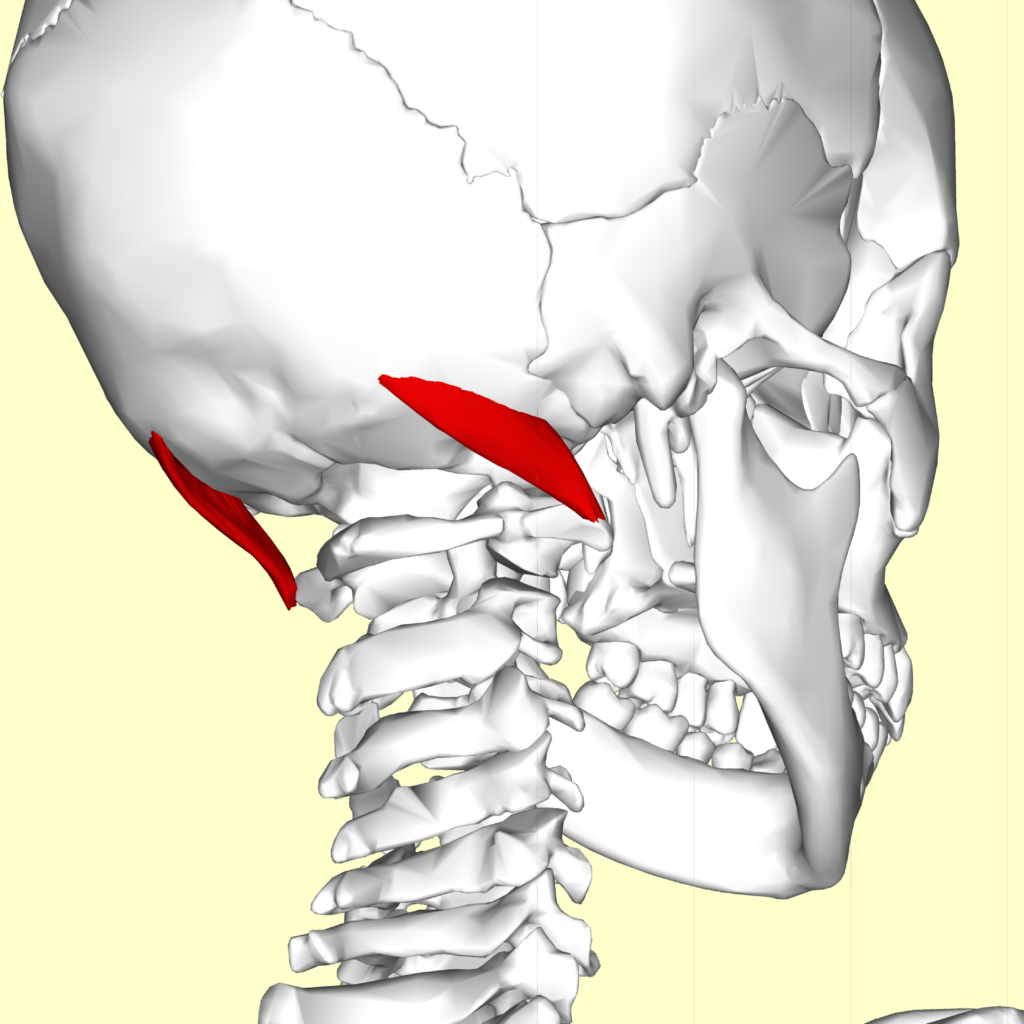
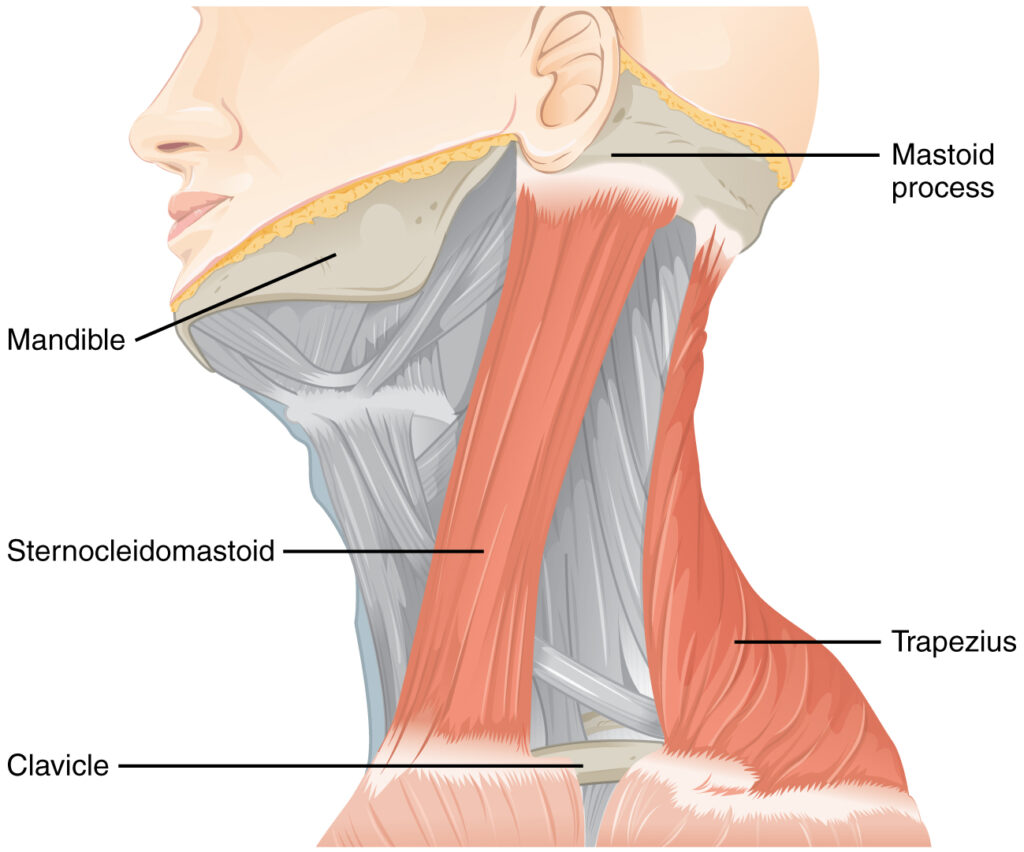
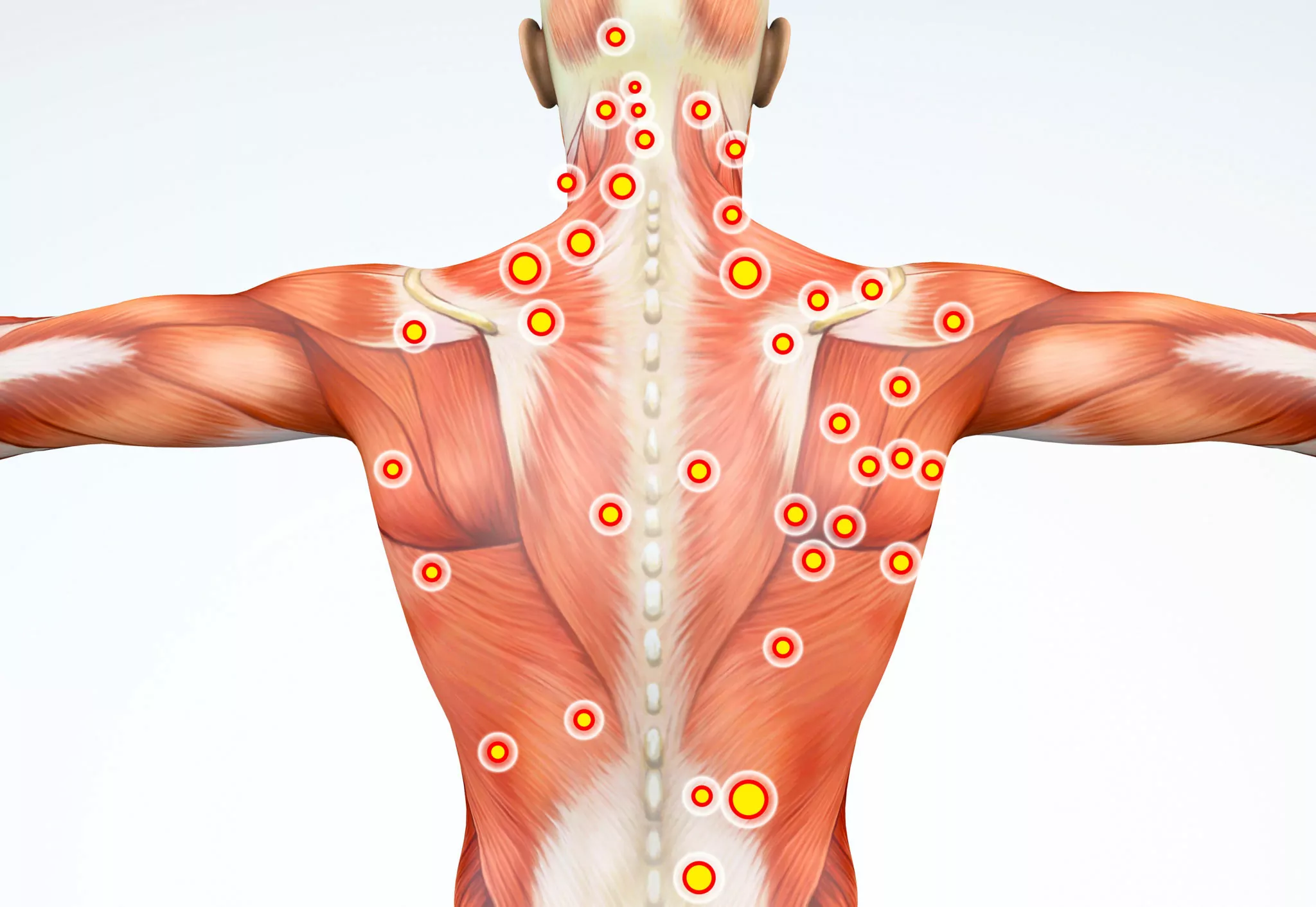
Treatment options for physical therapy include strength training, joint mobility, manual therapy and dry needling.
These interventions are generally safe, effective and can provide long-lasting relief. They also eliminate the risk of side effects that are often observed with medication. Often, medication side-effects make the use of that intervention undesirable. Taking medication can often lead to worsening or the development of unrelated, and previously not experienced symptoms. These can include dryness of eyes/mouth, gastro-intestinal and cardiovascular issues.
It is always recommended that you communicate to your health care provider the most accurate information regarding your symptoms, past and current treatments, effectiveness of those treatments, and your preference for any specific intervention.
If you are interested in pursuing non-pharmacological intervention, physical therapy may be the right choice for you.