Category: Uncategorized
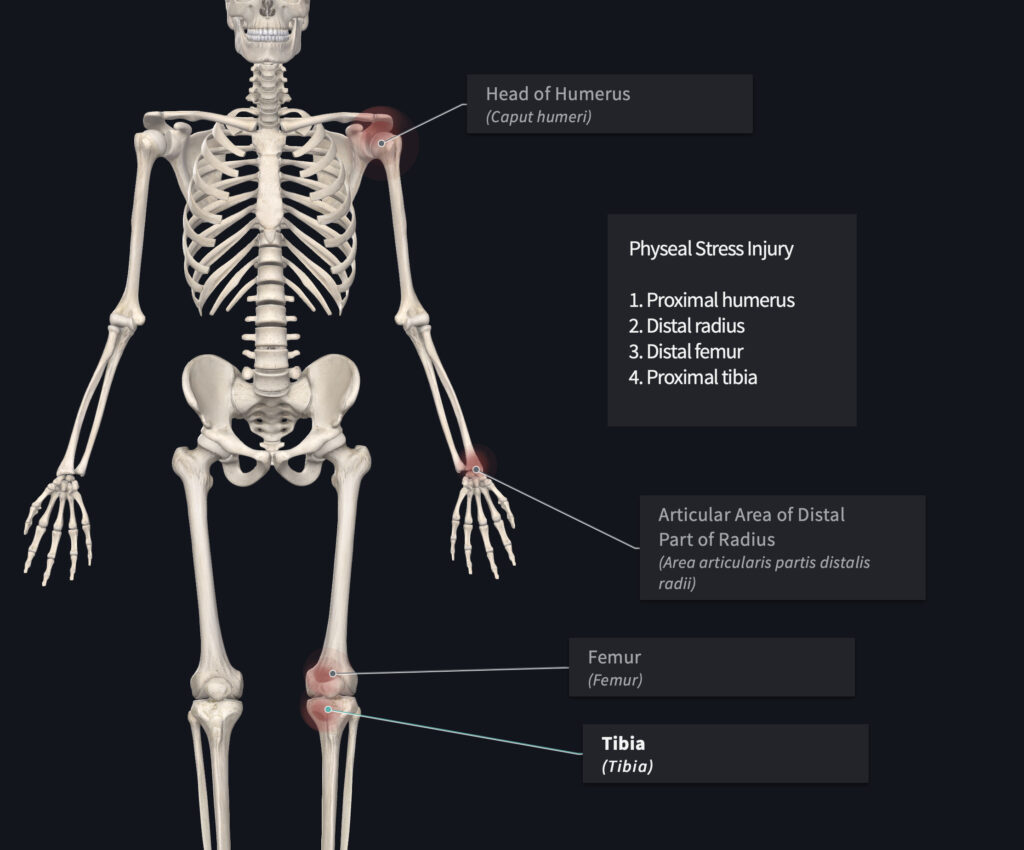
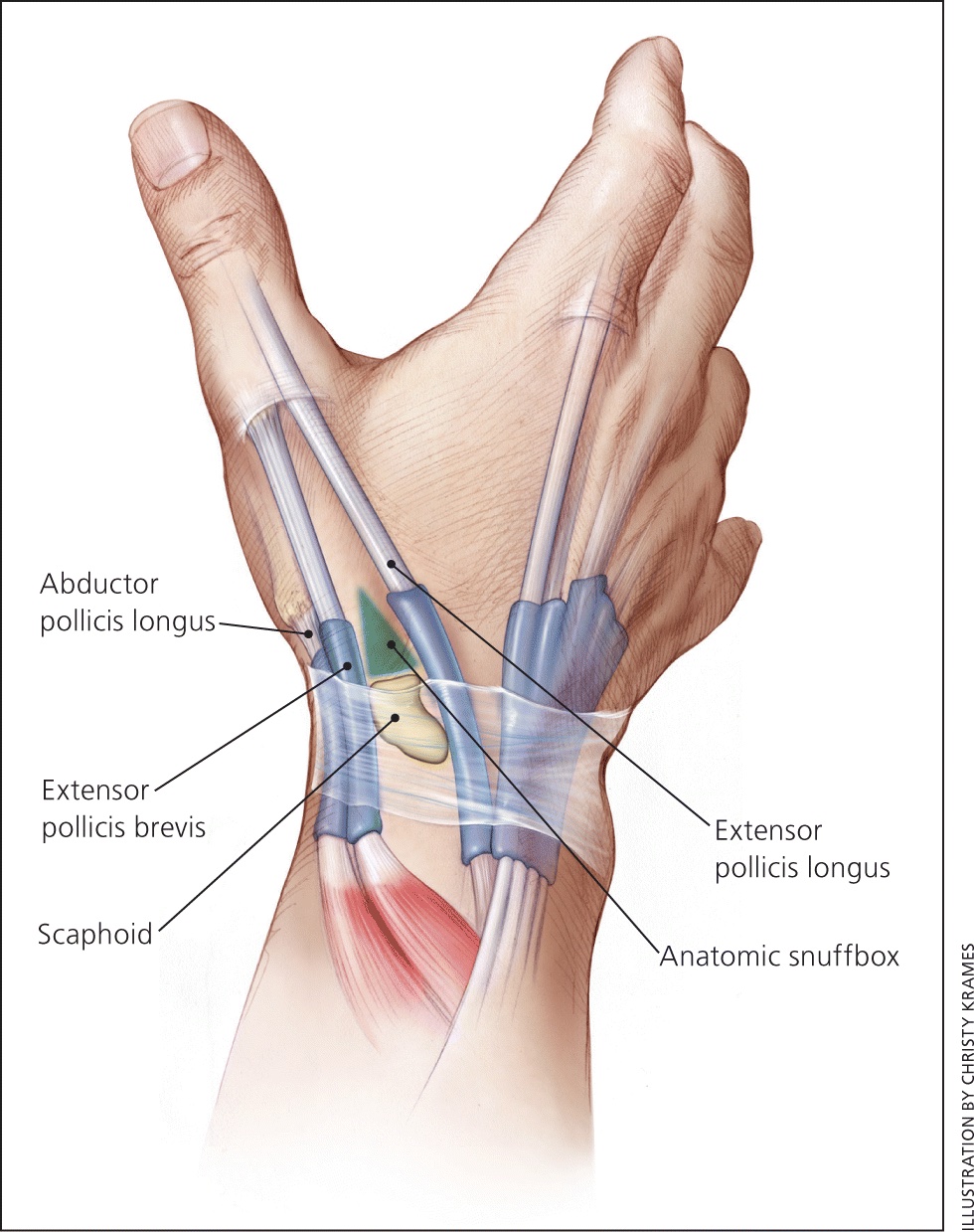
Shin (anterior tibia)
Tibial stress fractures have a high risk of nonunion. The “dreaded black line” may be observed on x-rays. If x-rays do not demonstrate a defect, MRI or CT scan may be warranted. Treatment requires a period of non-weightbearing and progressive return to sport. If nonoperative treatment fails, surgical intervention may be necessary.
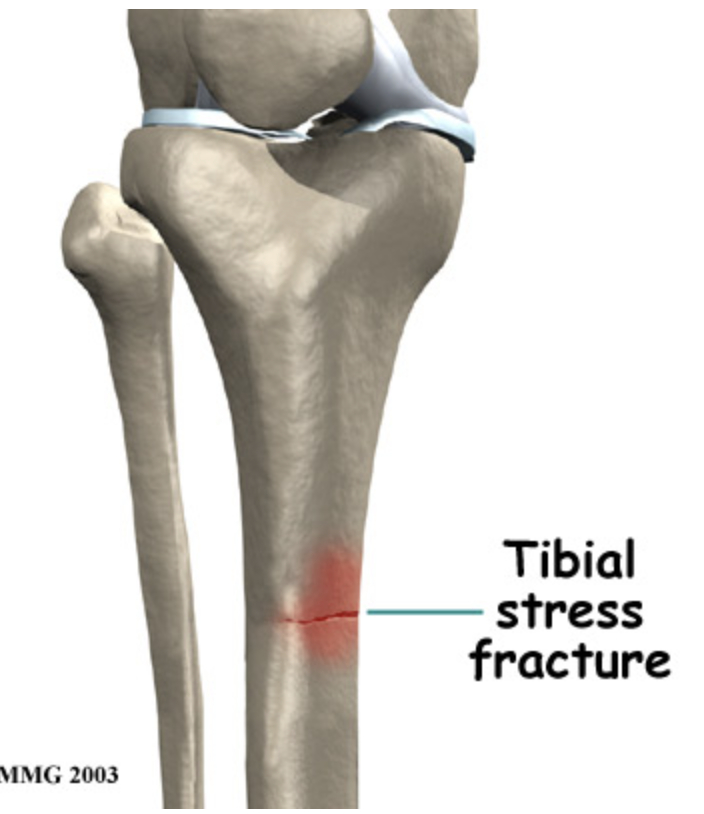
Ankle (medial malleolus)
Ankle stress fractures are uncommon in youth athletes. They are generally treated with rest and gradual return to sport. Stress fractures of the ankle are more common in bounding/jumping sports including gymnastics and dance. If the fracture progresses, surgical intervention may be required.
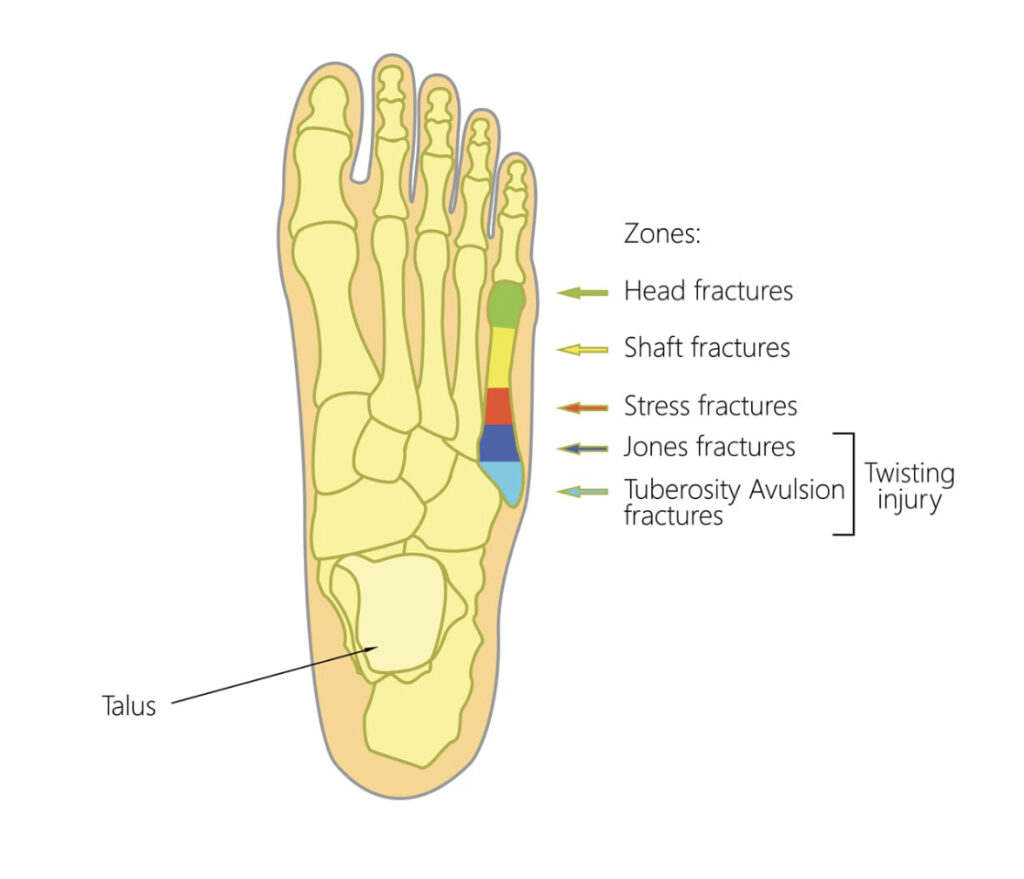
Foot (tarsal navicular stress fracture, fifth metatarsal stress fracture, sesamoid stress fracture)
Tarsal stress fractures are most prevalent in track and field, football and soccer. The most reliable method of identifying this type of fracture is a CT scan. There may be a delay in proper treatment due to the vague nature of complaints from the youth athlete. Poorly fitting footwear may contribute to the development and subsequent aggravation of the fracture.
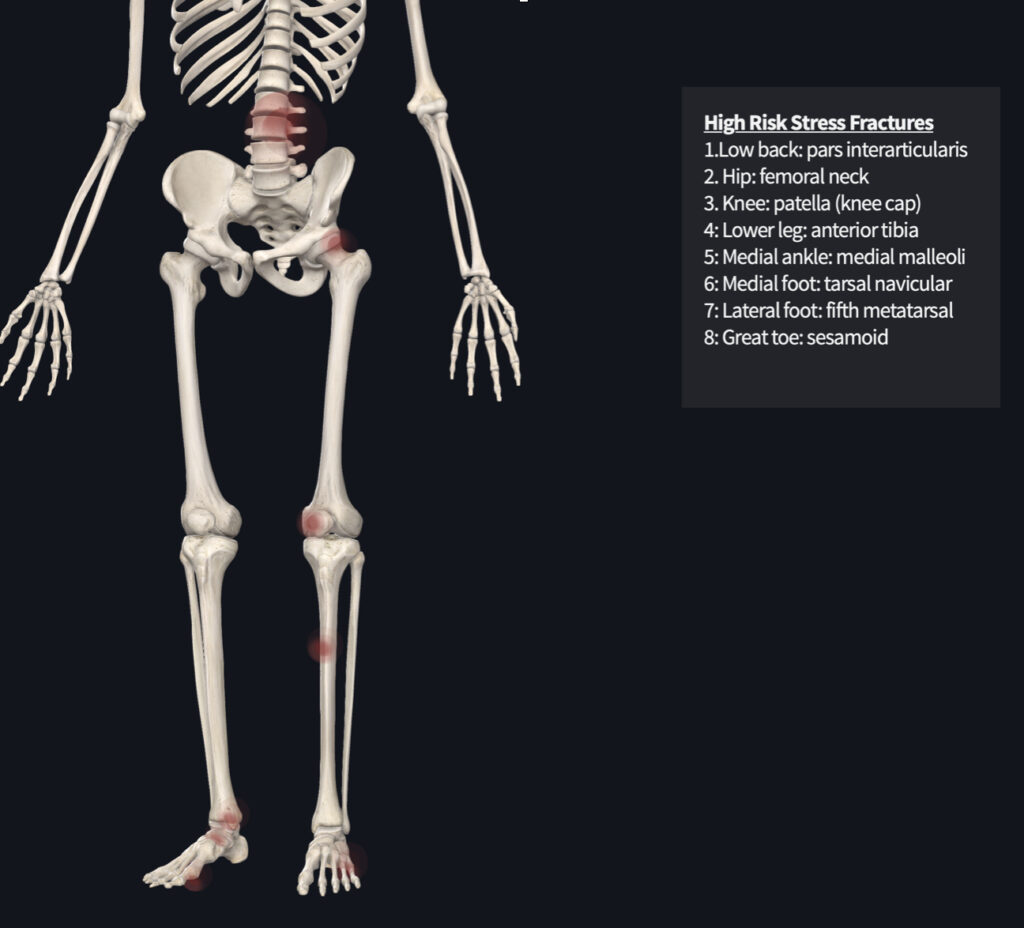
Clinical Clues for High-Risk Stress Fractures
Parents, coaches, athletes and health care providers should have a high index of suspicion when pain is reported at the site of high risk bone injuries. Localized tenderness over the site, coupled with the athletes history of onset of pain, should warrant imaging by a health care practitioner. Tenderness to touch of the spine and hip may not be reliable, thus, imaging should be done to rule out bony injury.
Radiographs (x-rays) may not be sensitive enough to identify stress reactions/fractures. Further imaging may be necessary (MRI, CT scan) to rule out bone injuries in youth athletes. Treatment of high risk stress reactions and fractures are specific to the site of injury. Very often, a period of rest (non-weightbearing) is required to allow the bone to heal. A progressive and graded return to sport may help prevent subsequent injury.
While there are no studies specific to prevention of stress fractures in youth athletes, the general consensus is similar to adults. Limiting high impact activities, optimizing vitamin D and calcium intake, screening for the female athlete triad and proper footwear should be assessed. Early recognition is key to optimal treatment.
If you are a youth athlete, parent of a youth athlete or coach youth athletics in Miami, Florida and have questions about information presented in this post, give our office a call. We offers seminars to educate the community on best practices for keeping youth athletes participating in sport. As a lifelong athlete myself, I can appreciate the time, effort and role parents and coaches can play in the development of their children. My goal is to keep as many people participating in athletics for as long as possible.