Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

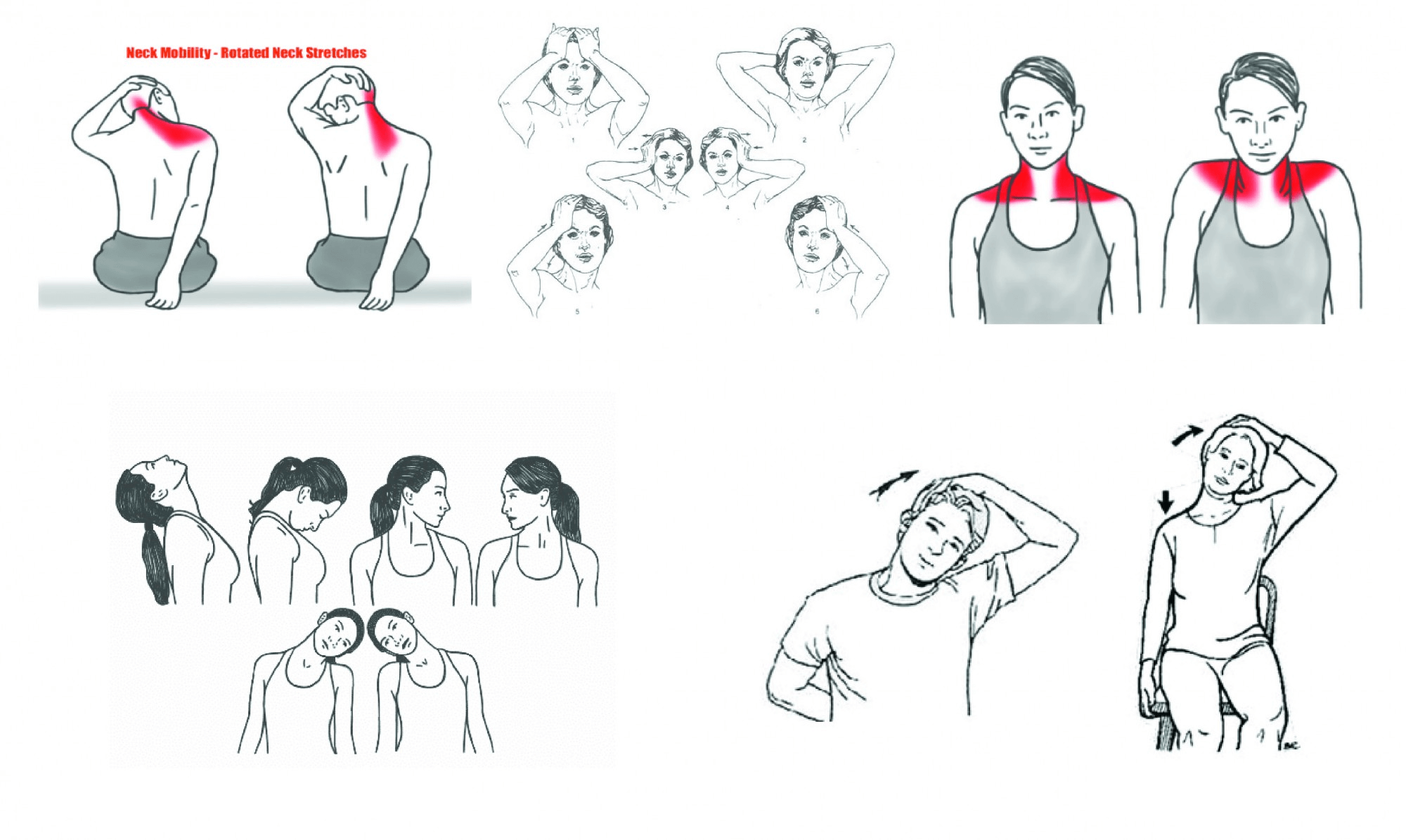
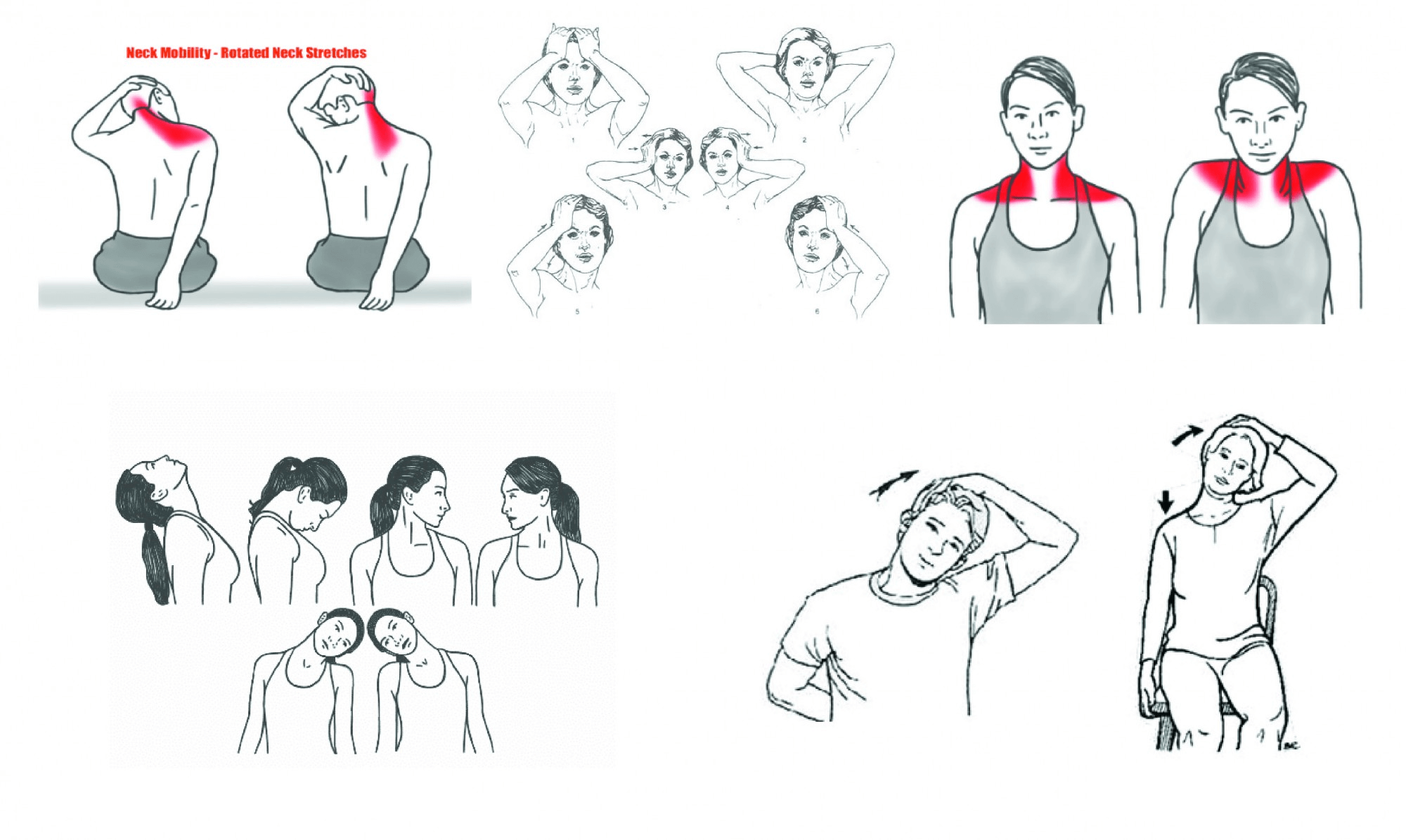
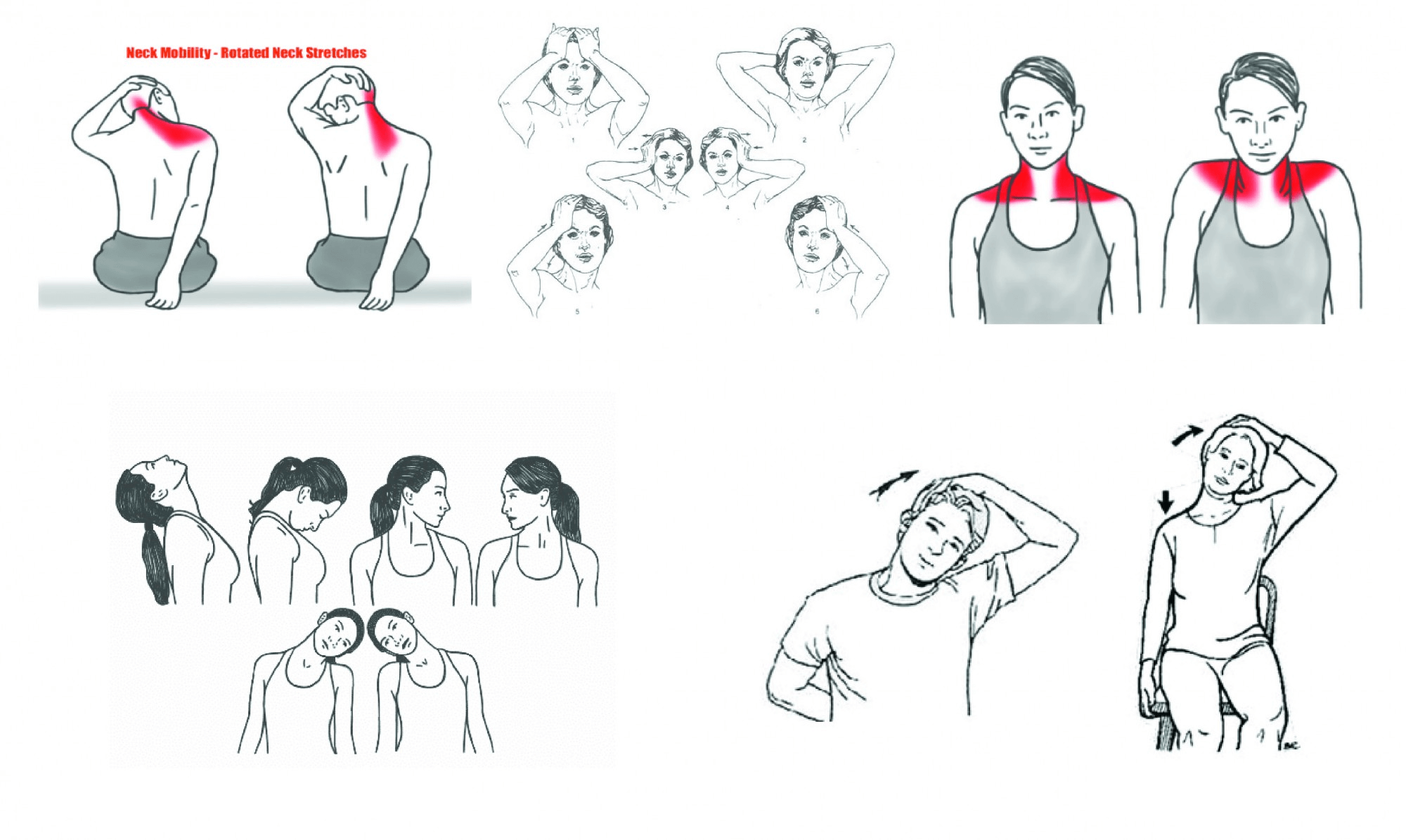
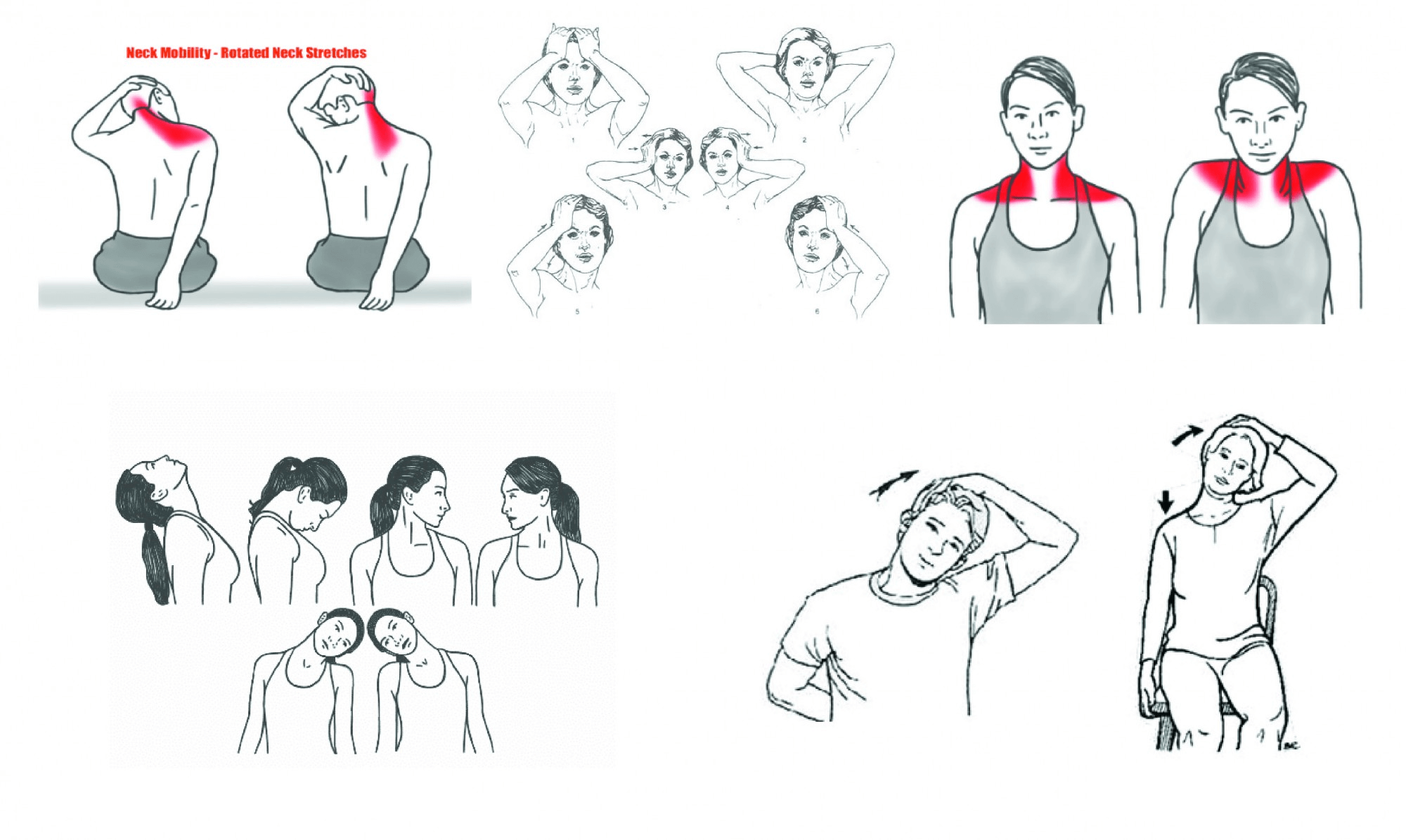
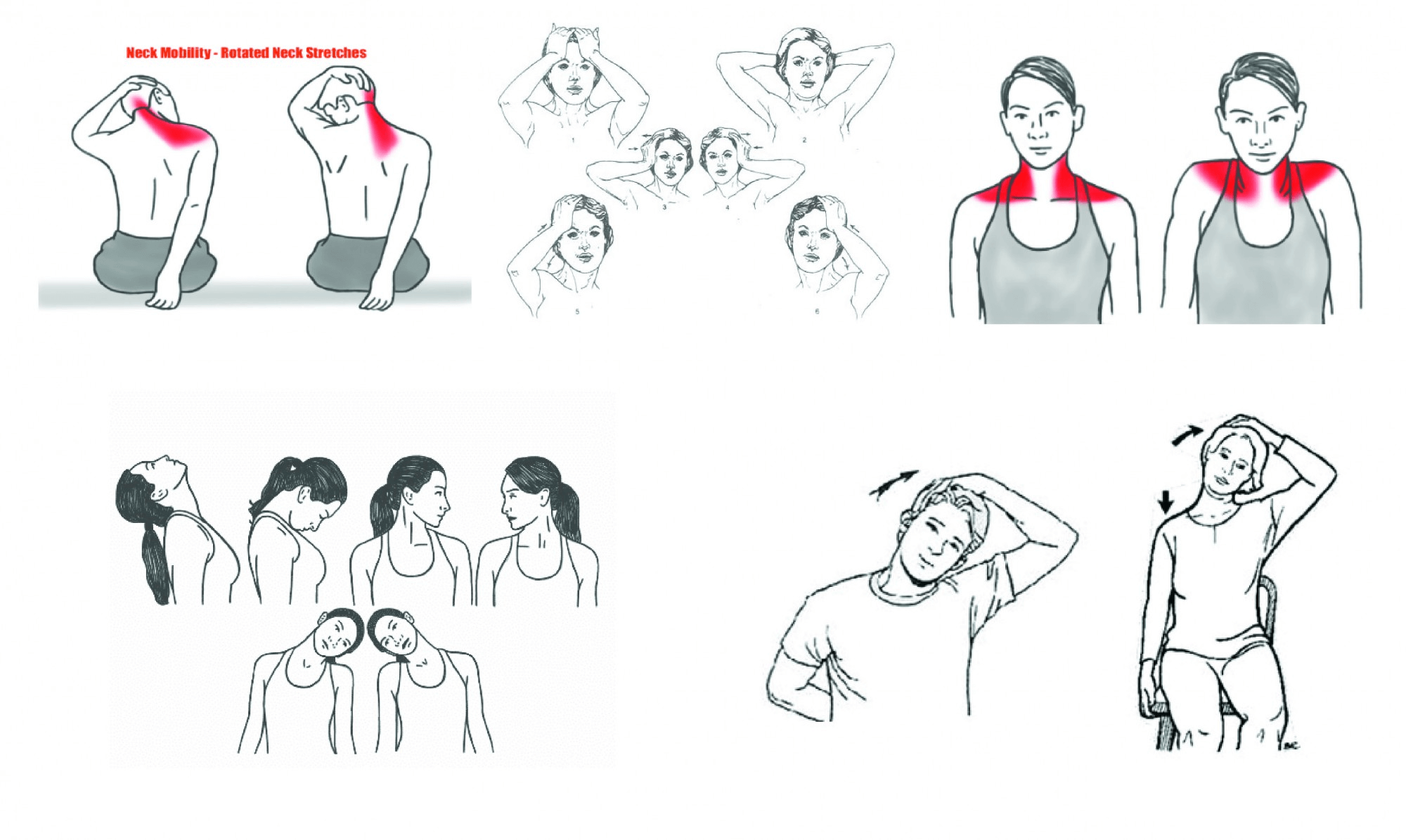
Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
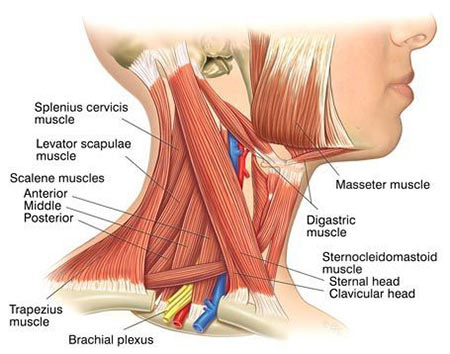
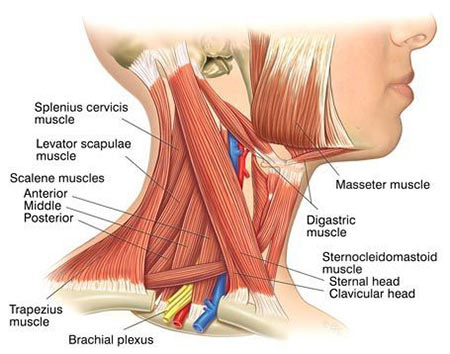
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
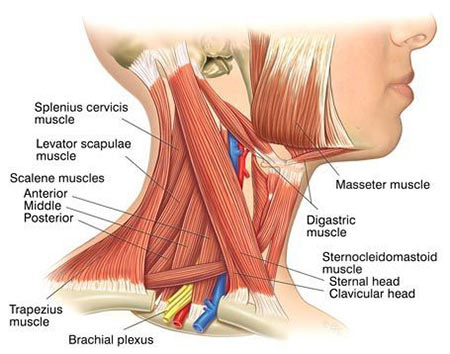
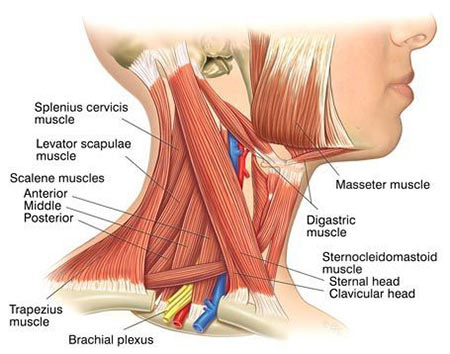
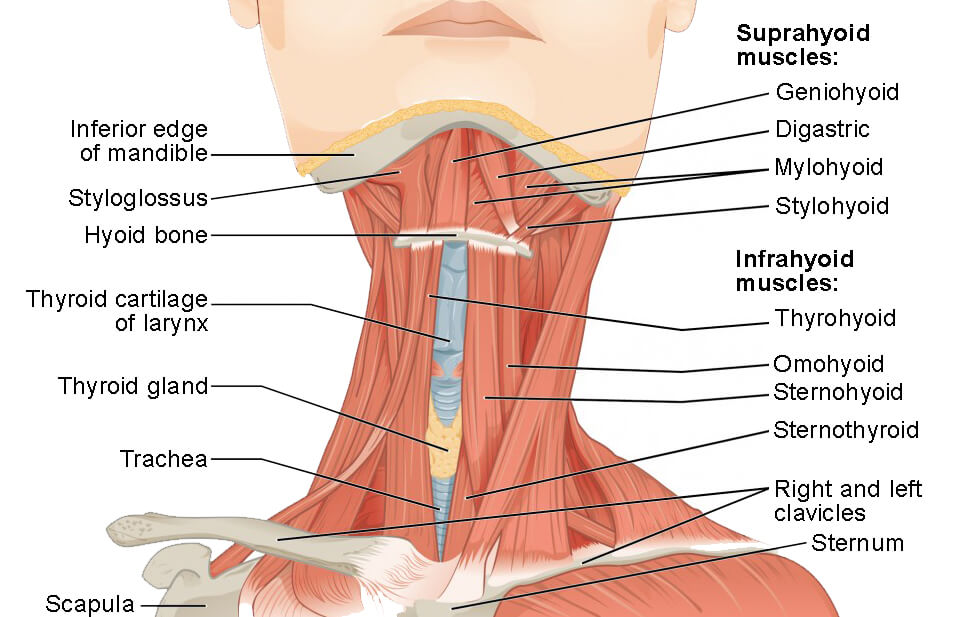
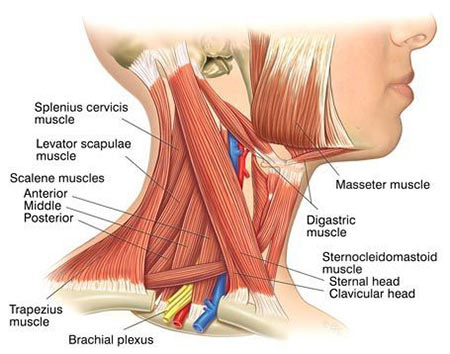
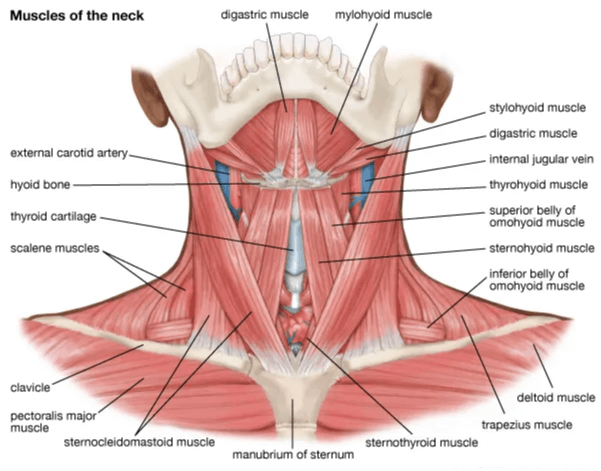
There are three types of neck muscles: anterior (front), posterior (back) and lateral (side) muscles.
Anterior neck muscles include:
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

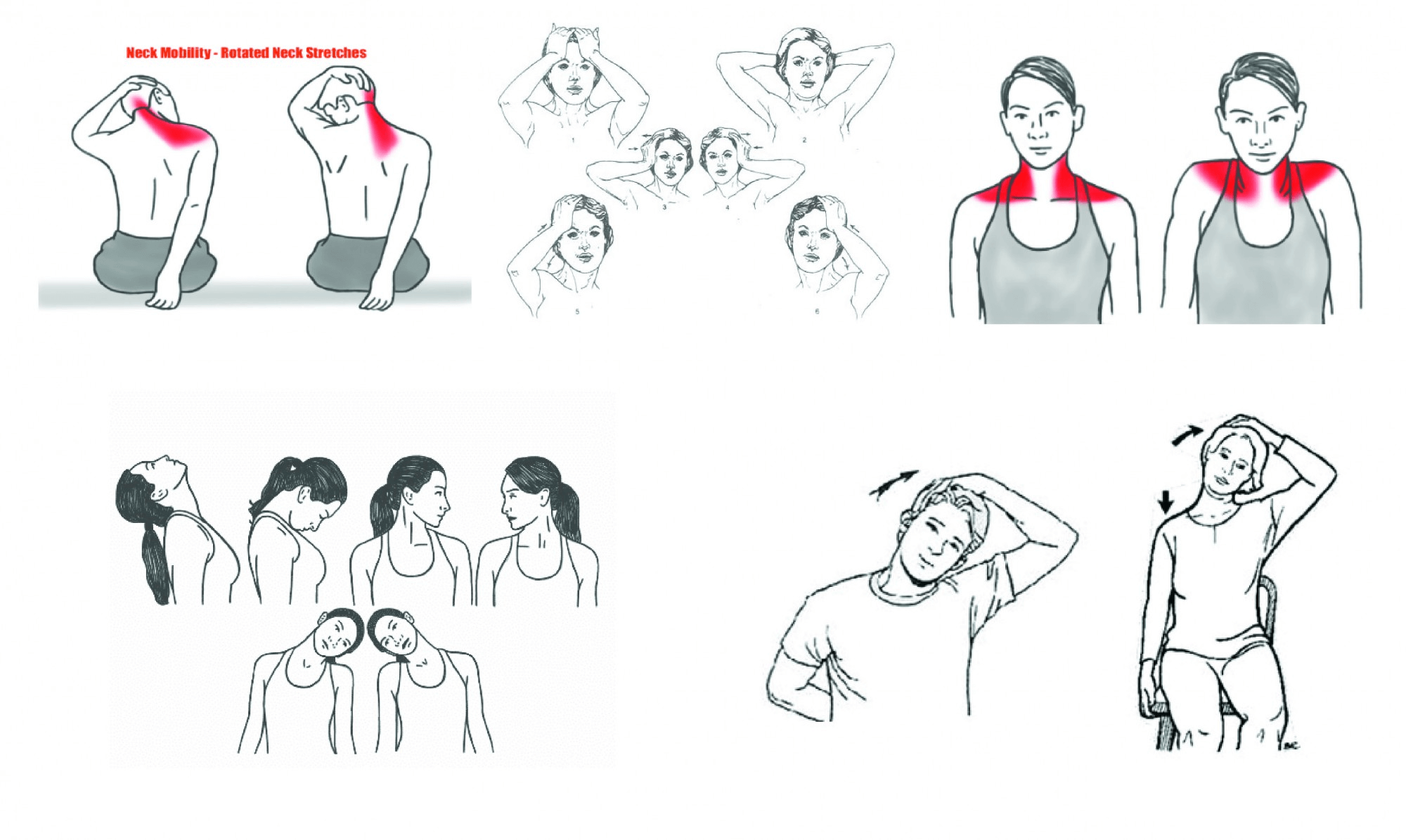
Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
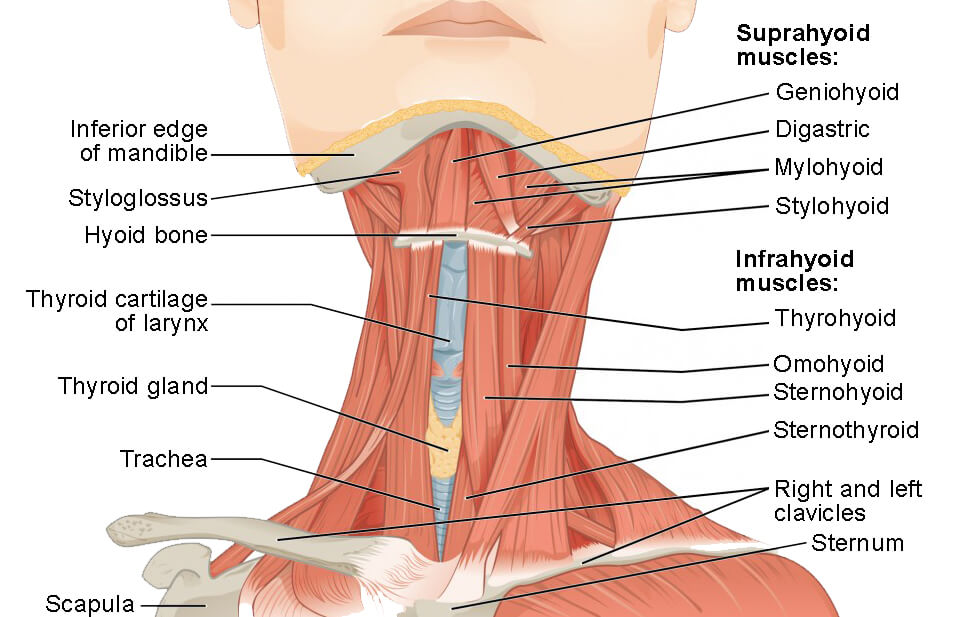
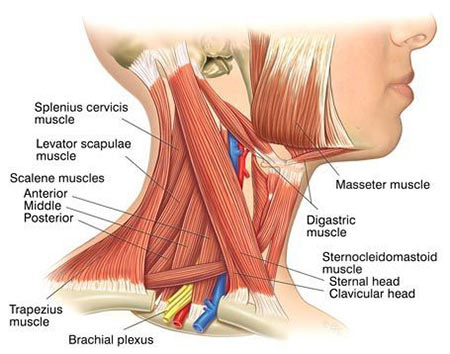
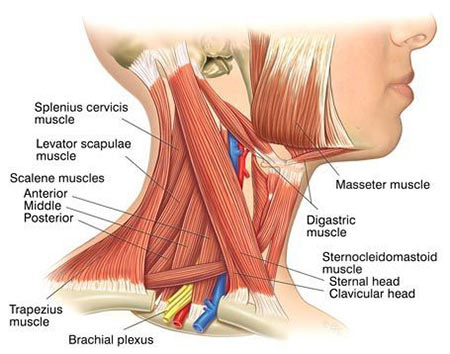
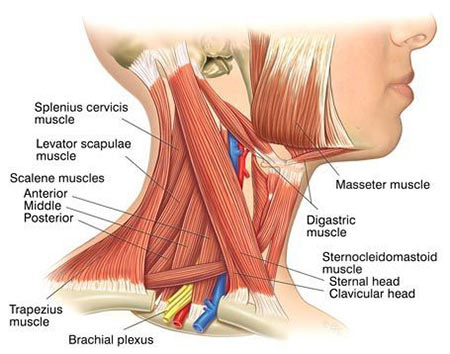
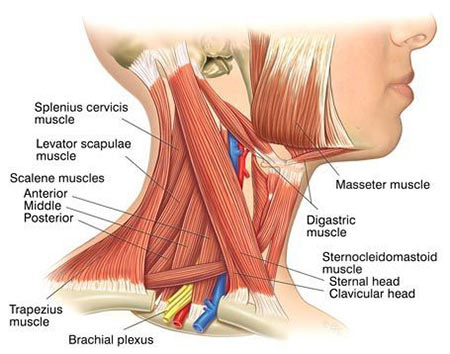
Your neck muscles are at the front, back and sides of your neck. From the back, they begin just beneath the base of your skull and extend down near the middle of your back, around your shoulder blades. From the front, these muscles begin at your jaw and extend to your collarbone at the top of your chest.
There are three types of neck muscles: anterior (front), posterior (back) and lateral (side) muscles.
Anterior neck muscles include:
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
The neck muscles serve a variety of functions, including:
Your neck muscles are at the front, back and sides of your neck. From the back, they begin just beneath the base of your skull and extend down near the middle of your back, around your shoulder blades. From the front, these muscles begin at your jaw and extend to your collarbone at the top of your chest.
There are three types of neck muscles: anterior (front), posterior (back) and lateral (side) muscles.
Anterior neck muscles include:
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Your neck muscles are part of a complex musculoskeletal system (soft tissues and bones) that connect the base of your skull to your torso. Muscles contain fibers that contract (get smaller), allowing you to perform lots of different movements. Your neck muscles help you do everything from chewing and swallowing to nodding your head. You have more than 20 neck muscles.
The muscles in your neck are skeletal muscles, meaning they’re attached to bones by tendons. They’re voluntary muscles, so you control how they move and work. Other types of muscles in the body – cardiac (in the heart) and smooth (in hollow organs like your stomach) – are involuntary, which means they work without you having to think about it.
The neck muscles serve a variety of functions, including:
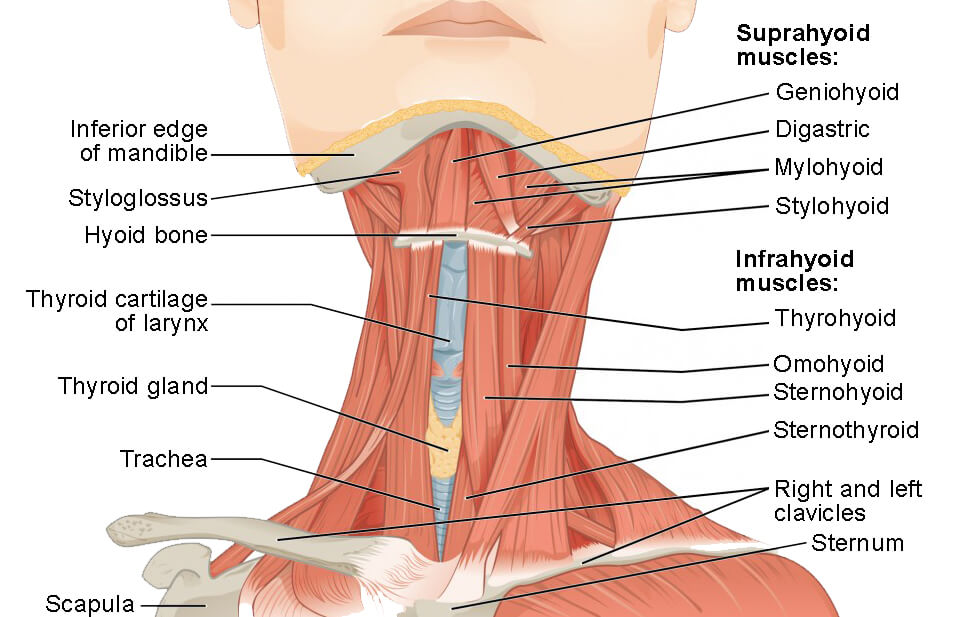
Your neck muscles are at the front, back and sides of your neck. From the back, they begin just beneath the base of your skull and extend down near the middle of your back, around your shoulder blades. From the front, these muscles begin at your jaw and extend to your collarbone at the top of your chest.
There are three types of neck muscles: anterior (front), posterior (back) and lateral (side) muscles.
Anterior neck muscles include:
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:

You have more than 20 neck muscles, extending from the base of your skull and jaw down to your shoulder blades and collarbone. These muscles support and stabilize your head, neck and the upper part of your spine. They help you move your head in different directions and assist with chewing, swallowing and breathing.
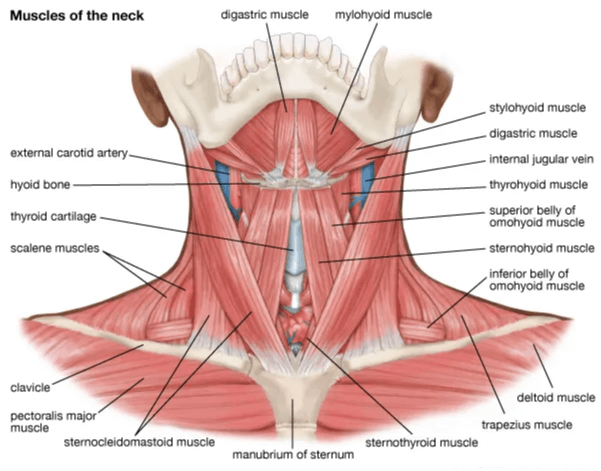
Your neck muscles are part of a complex musculoskeletal system (soft tissues and bones) that connect the base of your skull to your torso. Muscles contain fibers that contract (get smaller), allowing you to perform lots of different movements. Your neck muscles help you do everything from chewing and swallowing to nodding your head. You have more than 20 neck muscles.
The muscles in your neck are skeletal muscles, meaning they’re attached to bones by tendons. They’re voluntary muscles, so you control how they move and work. Other types of muscles in the body – cardiac (in the heart) and smooth (in hollow organs like your stomach) – are involuntary, which means they work without you having to think about it.
The neck muscles serve a variety of functions, including:
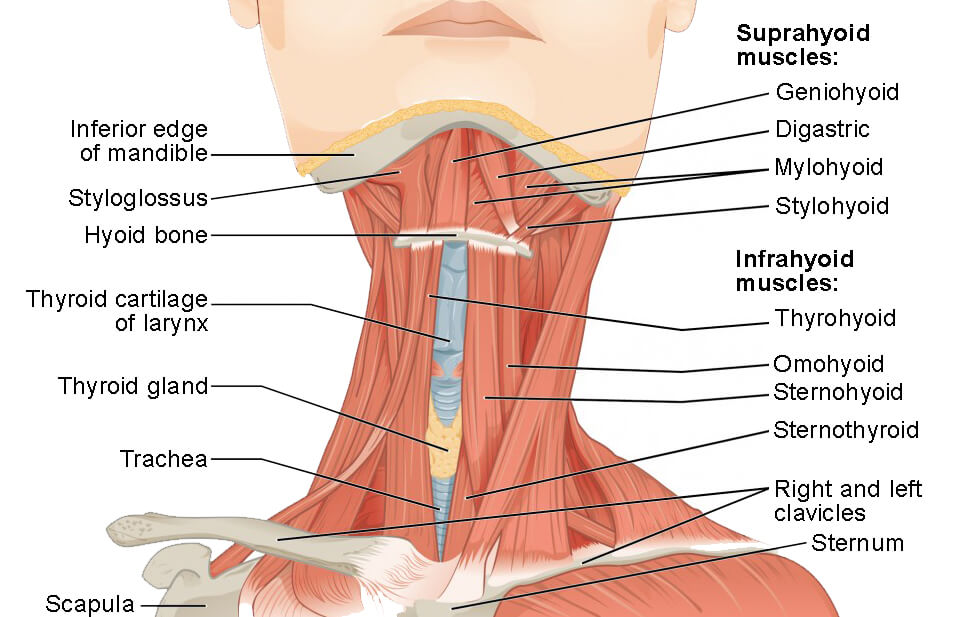
Your neck muscles are at the front, back and sides of your neck. From the back, they begin just beneath the base of your skull and extend down near the middle of your back, around your shoulder blades. From the front, these muscles begin at your jaw and extend to your collarbone at the top of your chest.
There are three types of neck muscles: anterior (front), posterior (back) and lateral (side) muscles.
Anterior neck muscles include:
Posterior neck muscles include:
Like all other skeletal muscles in the body, neck muscles contain lots of tiny, elastic fibers that allow the muscles to contract. Sheaths of tough connective tissue hold the fibers together. Skeletal muscle fibers are red and white, so the muscles look striated (striped or streaked).
Common conditions that affect the neck muscles include:
Studies estimate that about 14% of the population has some form of chronic neck pain. Approximately 45% of those cases (about 15.5 million Americans) may be due to whiplash.
Whiplash is typically the result of an automobile accident if you’re rear-ended. Neck injuries such as strains are common in athletes who play collision sports like football or hockey. But neck pain can happen to anyone. Turning your head suddenly, sleeping on your neck at an awkward angle, sitting at your desk with bad posture or other everyday activities can cause the occasional neck kink.
Neck injuries may cause:
Your healthcare provider reviews your symptoms and performs a physical exam. They may ask you to move your head, neck and shoulders in different directions to check your muscle strength and range of motion. Your provider may recommend imaging exams, such as an ultrasound or CT scan, if they think you may have muscle damage.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Keep your neck muscles strong and healthy by:
Serious neck injuries need immediate medical attention. Contact your doctor right away if you have:
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
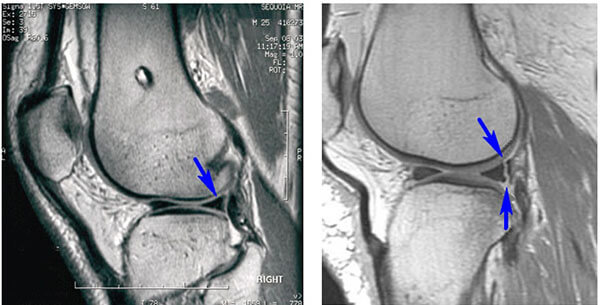
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
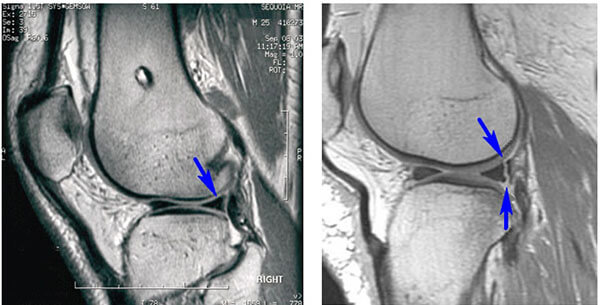
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
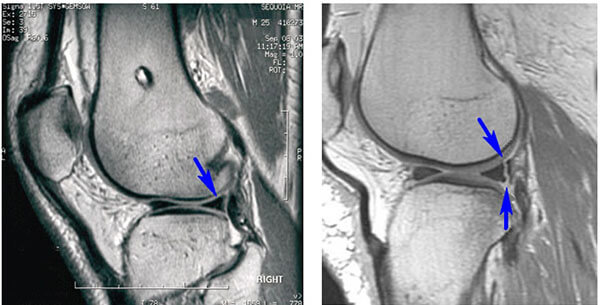
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
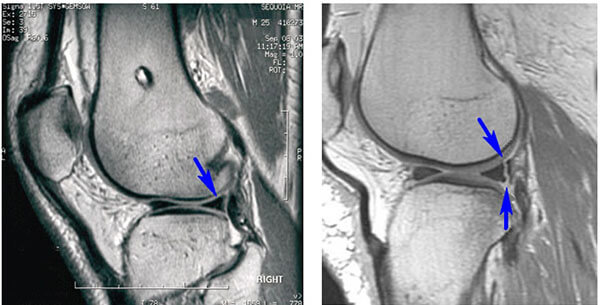
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
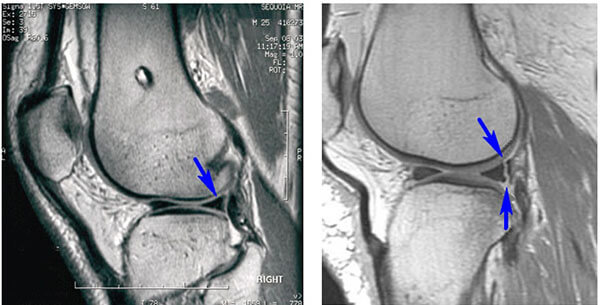
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
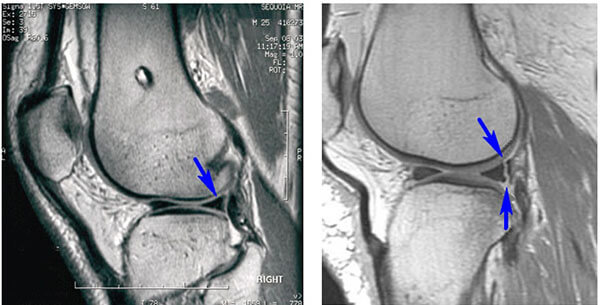
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
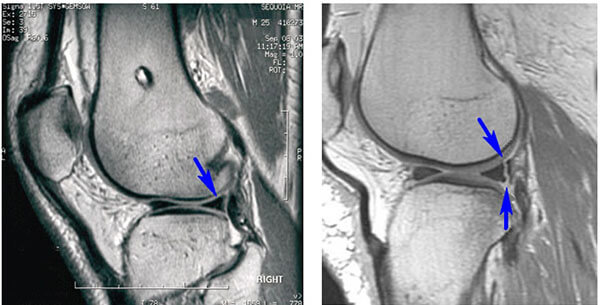
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
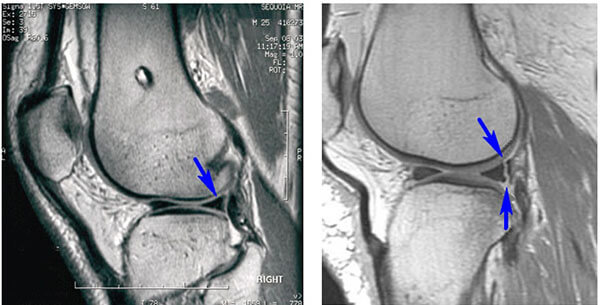
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
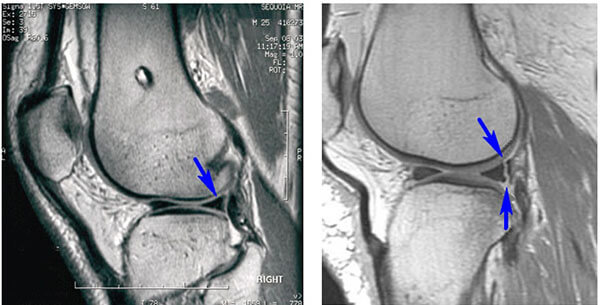
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
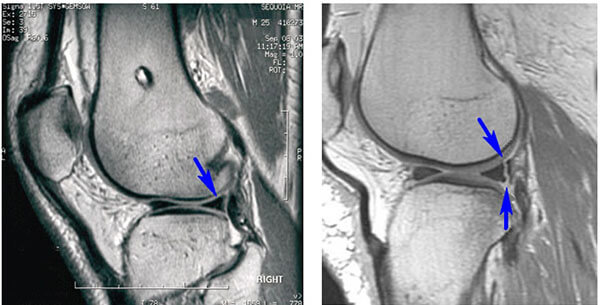
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
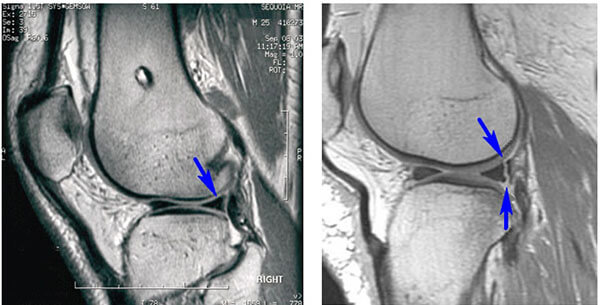
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
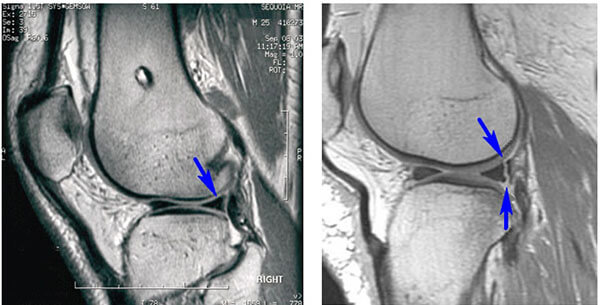
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
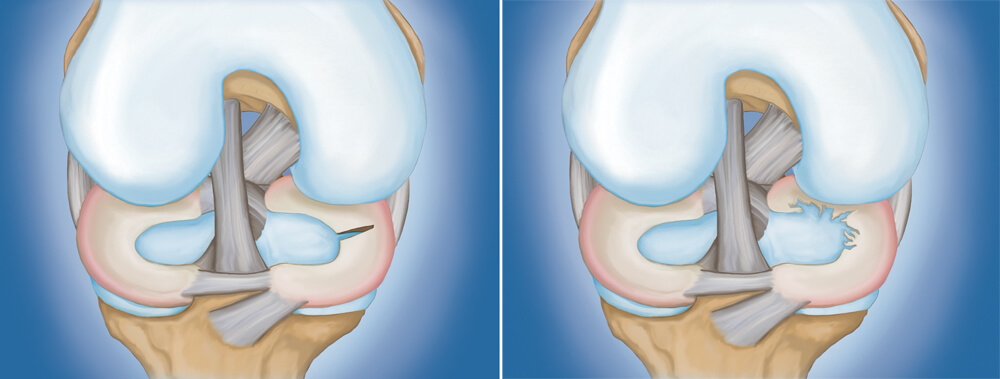
( (Left) Radial tear. (Right) Degenerative tear )
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
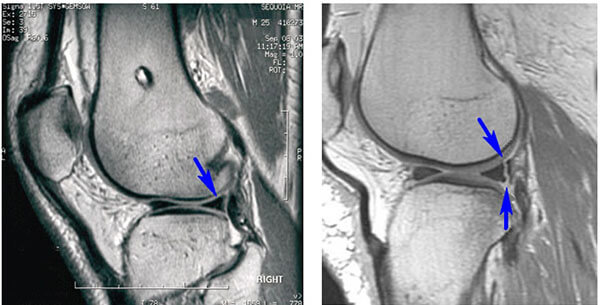
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
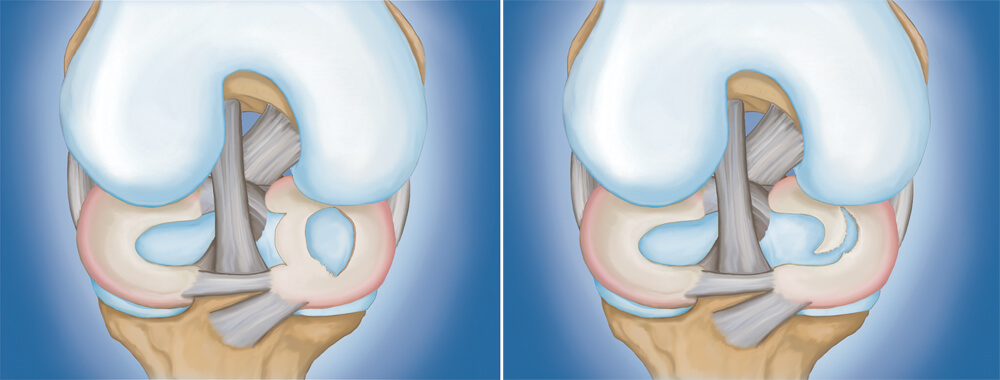
( Types of meniscus tears:
(Left) Bucket handle tear. (Right) Flap tear )
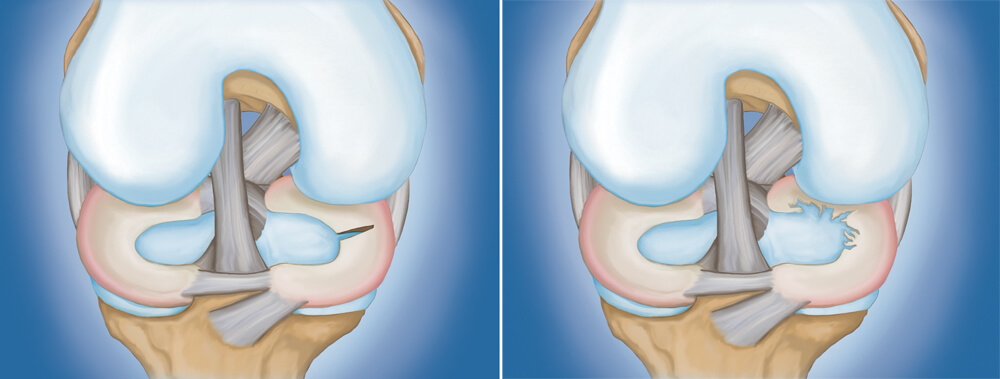
( (Left) Radial tear. (Right) Degenerative tear )
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
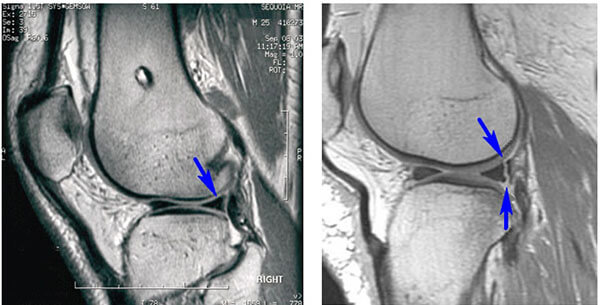
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
The meniscus can tear from acute trauma or as the result of degenerative changes that happen over time. Tears are noted by how they look, as well as where the tear occurs in the meniscus. Common tears include bucket handle, flap, and radial.
Sports-related meniscus injuries often occur along with other knee injuries, such as anterior cruciate ligament (ACL) tears.
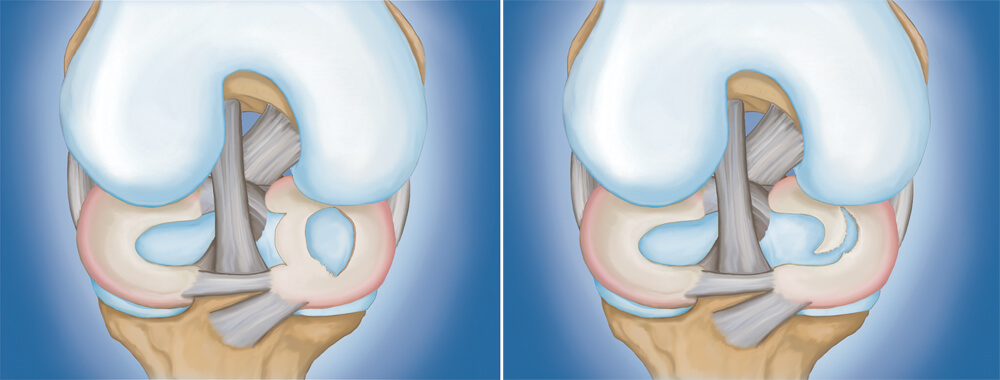
( Types of meniscus tears:
(Left) Bucket handle tear. (Right) Flap tear )
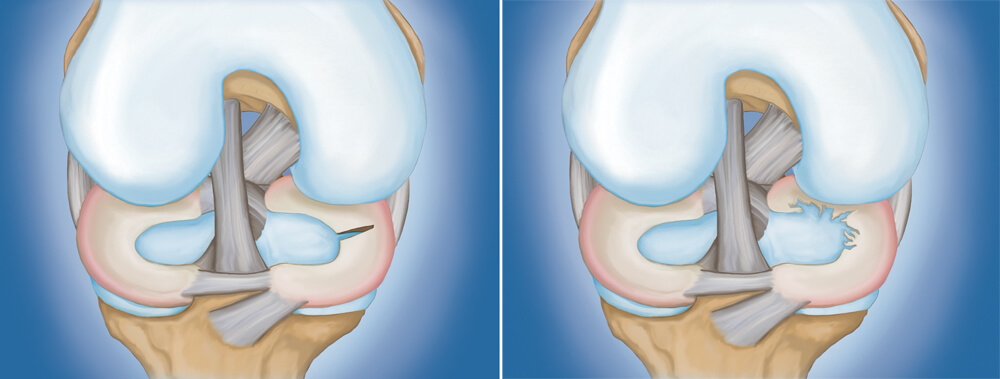
( (Left) Radial tear. (Right) Degenerative tear )
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
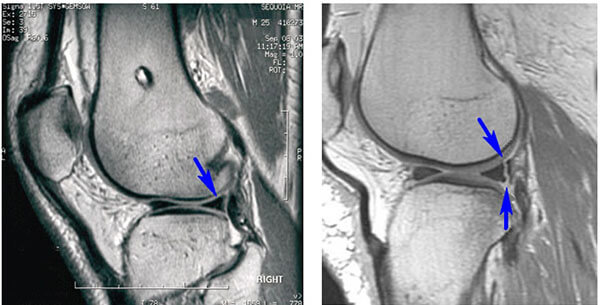
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
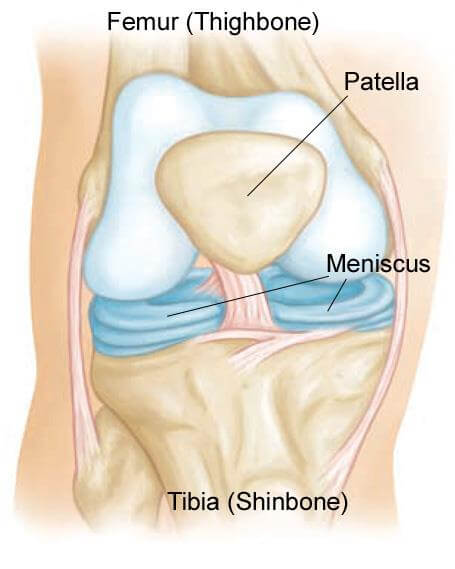
( Normal knee anatomy. The menisci are two rubbery disks that help cushion the knee joint )
The meniscus can tear from acute trauma or as the result of degenerative changes that happen over time. Tears are noted by how they look, as well as where the tear occurs in the meniscus. Common tears include bucket handle, flap, and radial.
Sports-related meniscus injuries often occur along with other knee injuries, such as anterior cruciate ligament (ACL) tears.
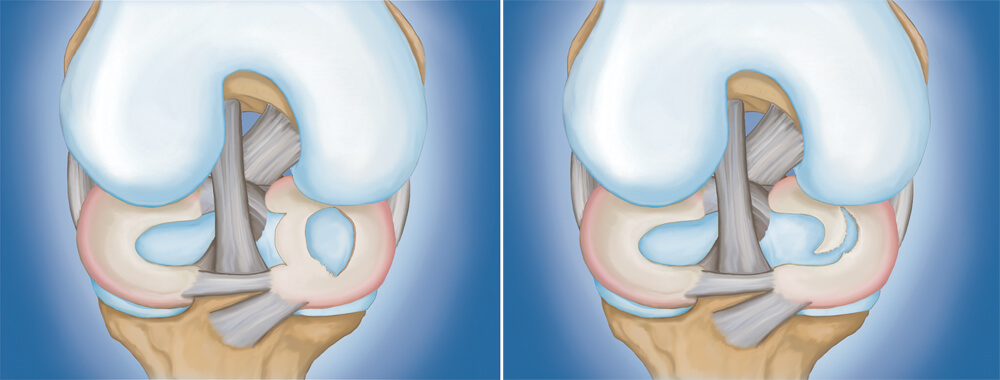
( Types of meniscus tears:
(Left) Bucket handle tear. (Right) Flap tear )
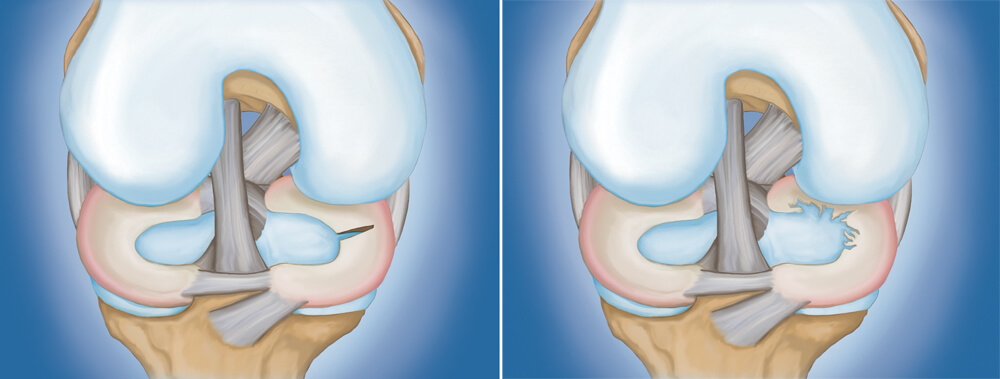
( (Left) Radial tear. (Right) Degenerative tear )
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
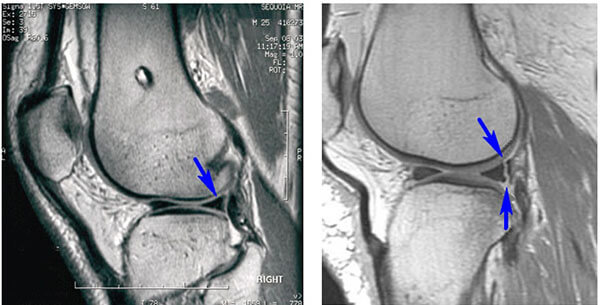
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
Two bones meet to form your knee joint: the femur and the tibia. The kneecap (patella) sits in front of the joint to provide some protection.
Two wedge-shaped pieces of fibrocartilage act as shock absorbers between your femur and tibia. These are the menisci. The menisci help to transmit weight from one bone to another and play an important role in knee stability.
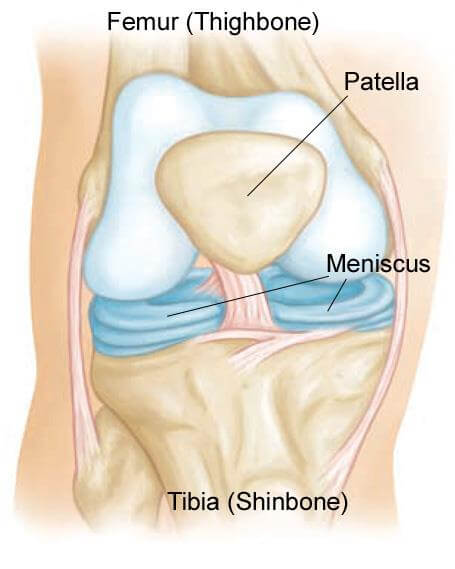
( Normal knee anatomy. The menisci are two rubbery disks that help cushion the knee joint )
The meniscus can tear from acute trauma or as the result of degenerative changes that happen over time. Tears are noted by how they look, as well as where the tear occurs in the meniscus. Common tears include bucket handle, flap, and radial.
Sports-related meniscus injuries often occur along with other knee injuries, such as anterior cruciate ligament (ACL) tears.
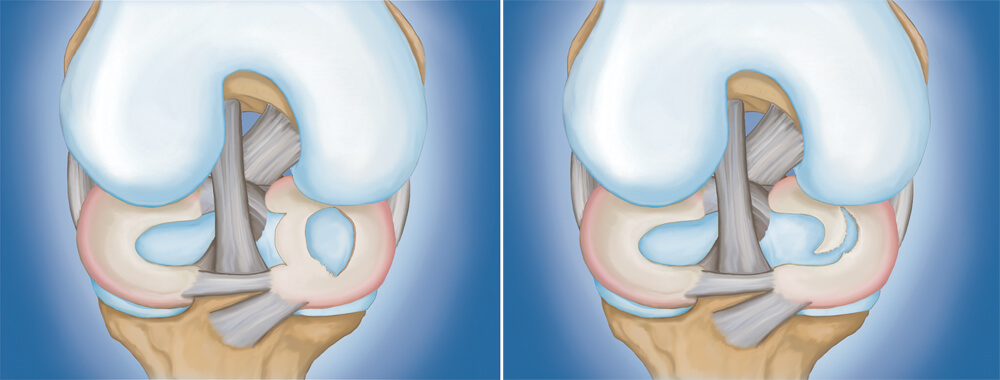
( Types of meniscus tears:
(Left) Bucket handle tear. (Right) Flap tear )
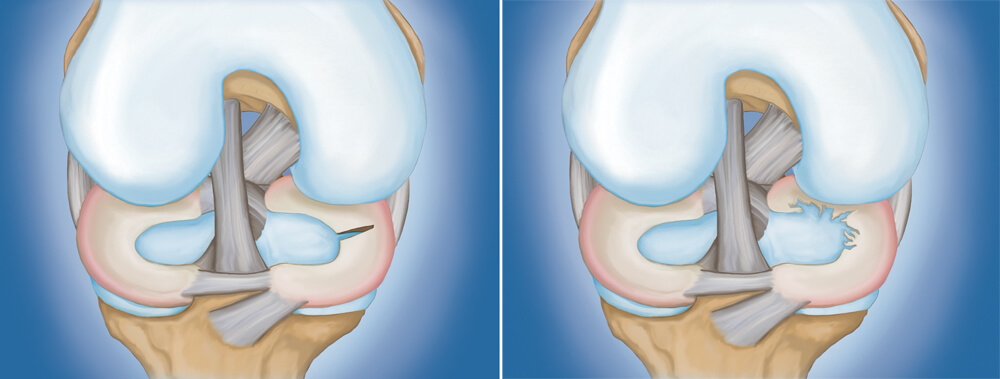
( (Left) Radial tear. (Right) Degenerative tear )
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
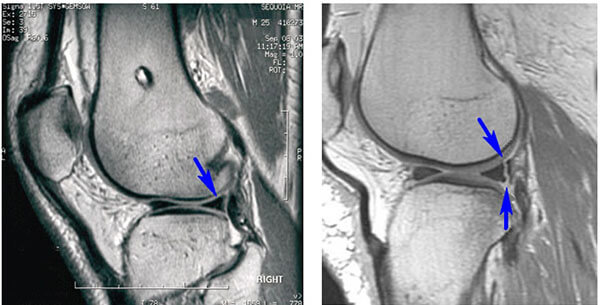
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.

Meniscus tears are among the most common knee injuries. Athletes, particularly those who play contact sports, are at risk for meniscus tears. However, anyone at any age can tear the meniscus. When people talk about torn cartilage in the knee, they are usually referring to a torn meniscus.
Two bones meet to form your knee joint: the femur and the tibia. The kneecap (patella) sits in front of the joint to provide some protection.
Two wedge-shaped pieces of fibrocartilage act as shock absorbers between your femur and tibia. These are the menisci. The menisci help to transmit weight from one bone to another and play an important role in knee stability.
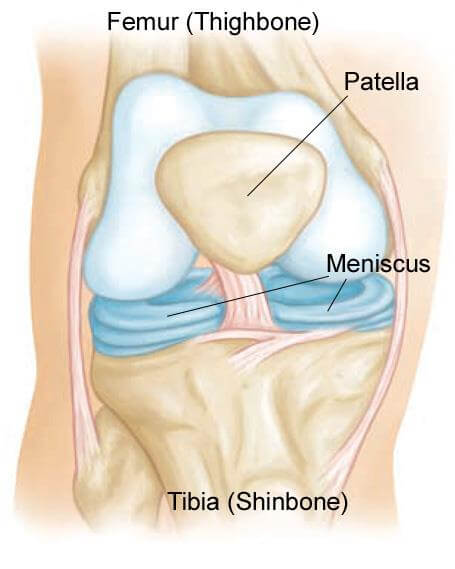
( Normal knee anatomy. The menisci are two rubbery disks that help cushion the knee joint )
The meniscus can tear from acute trauma or as the result of degenerative changes that happen over time. Tears are noted by how they look, as well as where the tear occurs in the meniscus. Common tears include bucket handle, flap, and radial.
Sports-related meniscus injuries often occur along with other knee injuries, such as anterior cruciate ligament (ACL) tears.
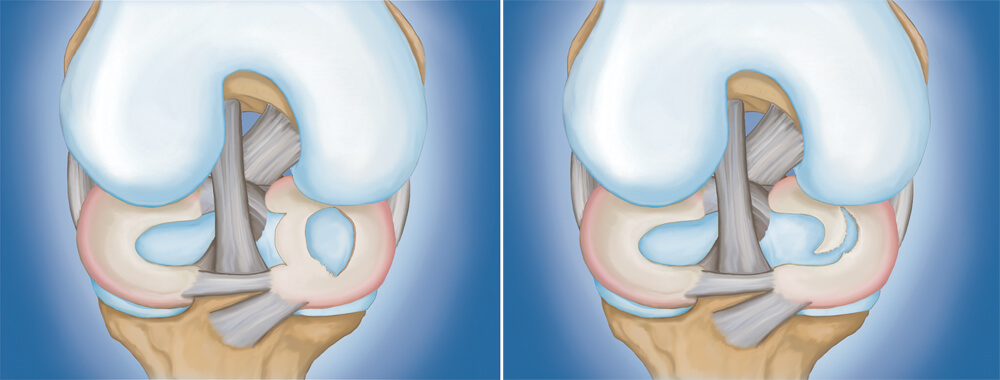
( Types of meniscus tears:
(Left) Bucket handle tear. (Right) Flap tear )
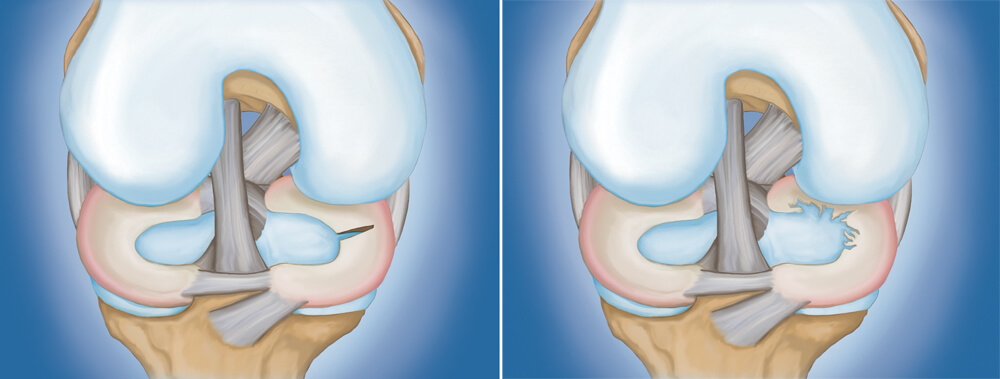
( (Left) Radial tear. (Right) Degenerative tear )
Acute meniscus tears often happen during sports. These can occur through either a contact or non-contact injury — for example, a pivoting or cutting injury.
As people age, they are more likely to have degenerative meniscus tears. Aged, worn tissue is more prone to tears. An awkward twist when getting up from a chair may be enough to cause a tear in an aging meniscus.
You might feel a pop when you tear the meniscus. Most people can still walk on their injured knee, and many athletes are able to keep playing with a tear. Over 2 to 3 days, however, the knee will gradually become more stiff and swollen.
The most common symptoms of a meniscus tear are:
After discussing your symptoms and medical history, your doctor will examine your knee. They will check for tenderness along the joint line where the meniscus sits. This often signals a tear.

( During the exam, your doctor will look for signs of tenderness along the joint line )
One of the main tests for meniscus tears is the McMurray test. Your doctor will bend your knee, then straighten and rotate it. This puts tension on a torn meniscus. If you have a meniscus tear, this movement may cause pain, clicking, or a clunking sensation within the joint.

( The McMurray test (shown here) will help your doctor determine if you have a meniscus tear )
Because other knee injuries can cause similar symptoms, your doctor may order imaging tests to help confirm the diagnosis.
X-rays. X-rays provide images of dense structures, such as bone. Although an X-ray will not show a meniscus tear, your doctor may order one to look for other causes of knee pain, such as osteoarthritis.
Magnetic resonance imaging (MRI) scans. An MRI scan assesses the soft tissues in your knee joint, including the menisci, cartilage, tendons, and ligaments.
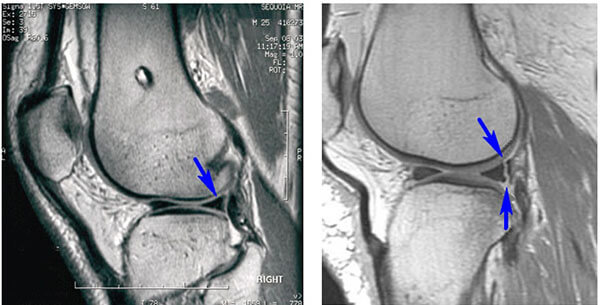
( MRI scans show (left) a normal meniscus and (right) a torn meniscus. The tear can be seen as a white line through the dark body of the meniscus )
The treatment your doctor recommends will depend on a number of factors, including your age, symptoms, and activity level. They will also consider the type, size, and location of the injury.
The outer one-third of the meniscus has a rich blood supply. A tear in this “red” zone may heal on its own, or can often be repaired with surgery. A longitudinal tear is an example of this kind of tear.
In contrast, the inner two-thirds of the meniscus lacks a significant blood supply. Without nutrients from blood, tears in this “white” zone with limited blood flow cannot heal. Because the pieces cannot grow back together, symptomatic tears in this zone that do not respond to conservative treatment are usually trimmed surgically.
Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs such as aspirin, ibuprofen, and naproxen help reduce pain and swelling.
Steroid injection. Your doctor may inject a corticosteroid medication into your knee joint to help eliminate pain and swelling.
Other nonsurgical treatment. Biologics injections, such as platelet-rich plasma (PRP), are currently being studied and may show promise in the future for the treatment of meniscus tears.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Procedure. Knee arthroscopy is one of the most commonly performed surgical procedures. In this procedure, the surgeon inserts a miniature camera through a small incision (portal) in the knee. This provides a clear view of the inside of the knee. The surgeon then inserts surgical instruments through two or three other small portals to trim or repair the tear.

( Illustration and photo show a camera and instruments inserted through portals in a knee )

( Close-up of partial meniscectomy )

( A torn meniscus repaired with sutures )
Once the initial healing is complete, your doctor will prescribe rehabilitation exercises. Regular exercise to restore your knee mobility and strength is necessary. You will start with exercises to improve your range of motion. Strengthening exercises will gradually be added to your rehabilitation plan.
In many cases, rehabilitation can be carried out at home, although your doctor may recommend working with a physical therapist. Rehabilitation time for a meniscus repair is about 3 to 6 months. A meniscectomy requires less time for healing — approximately 3 to 6 weeks.
Meniscus tears are extremely common knee injuries. With proper diagnosis, treatment, and rehabilitation, patients often return to their pre-injury abilities.
Activity modification: limit exposure to symptom provoking activity.
The primary goal of initial injury management is to manage symptoms. This may include avoidance of rapid movements, heavy lifting or dynamic/uncontrolled situations.
If you are an athlete, other options may include reducing overall workload or intensity of exercise, and limiting range of motion.
Oftentimes, athlete may become fear avoidant of performing a movement similar to the one that caused the injury. This, other goals may include improving confidence with movement. This can be achieved by the above mentioned recommendations.
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
Elbow injuries usually affect either the inner or outer elbow, and fall into three categories: soft tissue injuries (tendons, muscles, ligaments), bone injuries (fractures or osteoarthritis), or nerve injuries.
The most common elbow injuries seen by orthopedists and surgeons include the following:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
Elbow injuries usually affect either the inner or outer elbow, and fall into three categories: soft tissue injuries (tendons, muscles, ligaments), bone injuries (fractures or osteoarthritis), or nerve injuries.
The most common elbow injuries seen by orthopedists and surgeons include the following:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
Elbow injuries usually affect either the inner or outer elbow, and fall into three categories: soft tissue injuries (tendons, muscles, ligaments), bone injuries (fractures or osteoarthritis), or nerve injuries.
The most common elbow injuries seen by orthopedists and surgeons include the following:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
Throwing sports like football and baseball are particularly infamous for causing injuries along the inner side of the elbow.
However, you may also injure your elbow playing the following:
Elbow injuries usually affect either the inner or outer elbow, and fall into three categories: soft tissue injuries (tendons, muscles, ligaments), bone injuries (fractures or osteoarthritis), or nerve injuries.
The most common elbow injuries seen by orthopedists and surgeons include the following:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:

Most elbow injuries that bring people to the doctor are caused by repetitive strain, either from athletic injuries or other forms of overuse.
Repetitive strain injuries occur when you repeat an activity over and over again, with little time off between sessions to allow the body to heal. Over time, the joints or muscles involved in the activity can become inflamed or aggravated due to overuse. Symptoms like pain, swelling, stiffness, or weakness may begin gradually and worsen over time.
Among athletes, overhand throwers who use significant force and speed are the ones most likely to complain of elbow injury (think baseball pitchers or football players).
However, many different activities and sports can cause repetitive strain damage:
Throwing sports like football and baseball are particularly infamous for causing injuries along the inner side of the elbow.
However, you may also injure your elbow playing the following:
Elbow injuries usually affect either the inner or outer elbow, and fall into three categories: soft tissue injuries (tendons, muscles, ligaments), bone injuries (fractures or osteoarthritis), or nerve injuries.
The most common elbow injuries seen by orthopedists and surgeons include the following:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:

The elbow joint is a synovial (fluid-filled) hinge joint with several important functions: moving your hand toward and away from your body, rotating your forearm, and flexing and extending the arm (bending and straightening the elbow). To make all this movement happen, your joint consists of bones, cartilage, ligaments, and fluid. Any one of these can be harmed from overuse, leading to injury.

Most elbow injuries that bring people to the doctor are caused by repetitive strain, either from athletic injuries or other forms of overuse.
Repetitive strain injuries occur when you repeat an activity over and over again, with little time off between sessions to allow the body to heal. Over time, the joints or muscles involved in the activity can become inflamed or aggravated due to overuse. Symptoms like pain, swelling, stiffness, or weakness may begin gradually and worsen over time.
Among athletes, overhand throwers who use significant force and speed are the ones most likely to complain of elbow injury (think baseball pitchers or football players).
However, many different activities and sports can cause repetitive strain damage:
Throwing sports like football and baseball are particularly infamous for causing injuries along the inner side of the elbow.
However, you may also injure your elbow playing the following:
Elbow injuries usually affect either the inner or outer elbow, and fall into three categories: soft tissue injuries (tendons, muscles, ligaments), bone injuries (fractures or osteoarthritis), or nerve injuries.
The most common elbow injuries seen by orthopedists and surgeons include the following:
Tennis elbow usually announces itself with a weaker-than-normal grip strength and a painful soreness or burning in the outside of the elbow.
You need not play tennis to develop tennis elbow. Many people are surprised to hear that they can sustain the same injury from a variety of different activities that strain the tendons in a similar fashion (for example, doing yard work, swimming, or even typing).

Elbow pain may also be caused by:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:
If your elbow pain doesn’t respond to at-home treatments, you may need to see an orthopedist for a treatment program that’s somewhere between self-care and surgery. For example, your injury may respond to the following:
If your pain is severe, if you’re feeling numbness in the arm or hands, or if your sports performance and range of motion are suffering, you may want to consider elbow surgery. Making an appointment to see an orthopedist is the first step in determining whether a surgical option may benefit you.
Many orthopedists — including Coastal Orthopedics — specialize in elbow surgery.
Common elbow procedures include:

Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

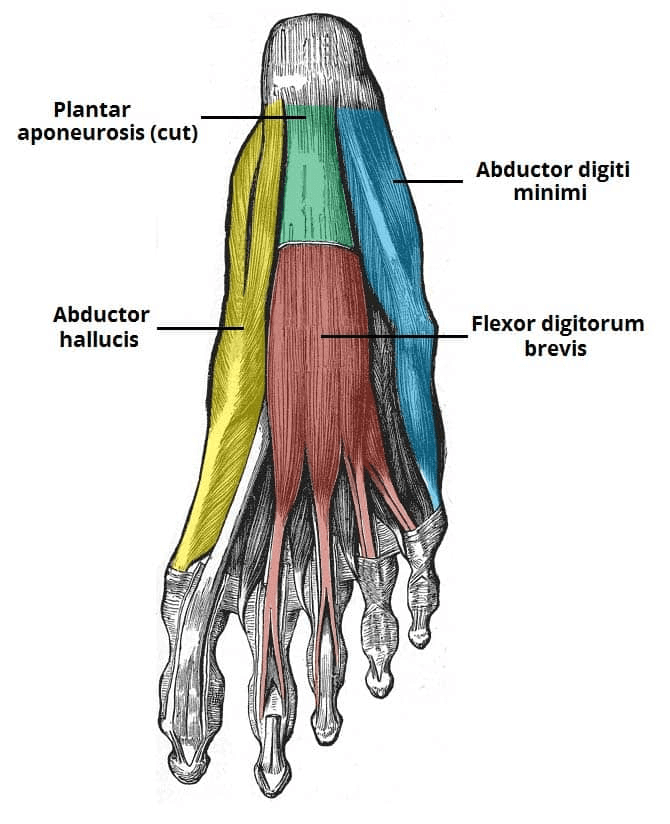
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

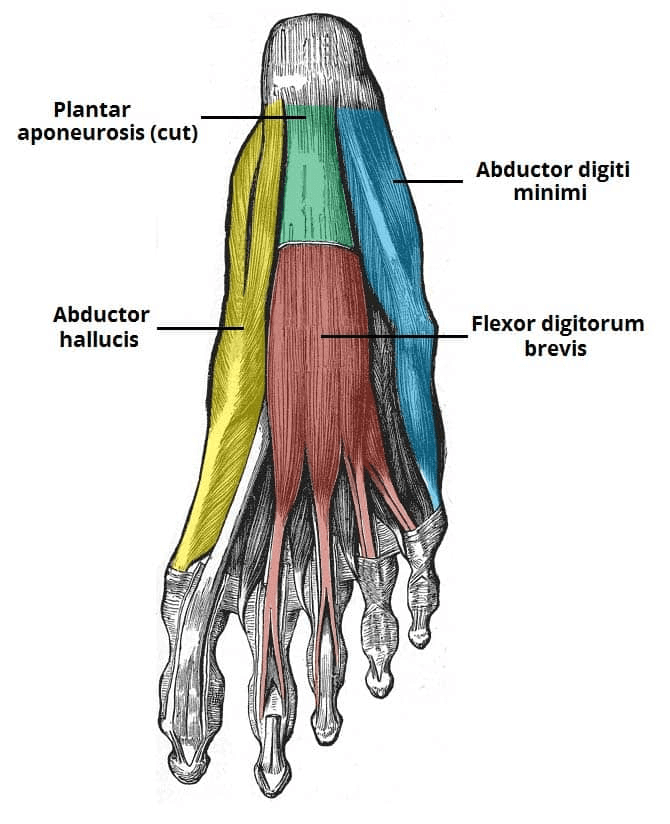
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
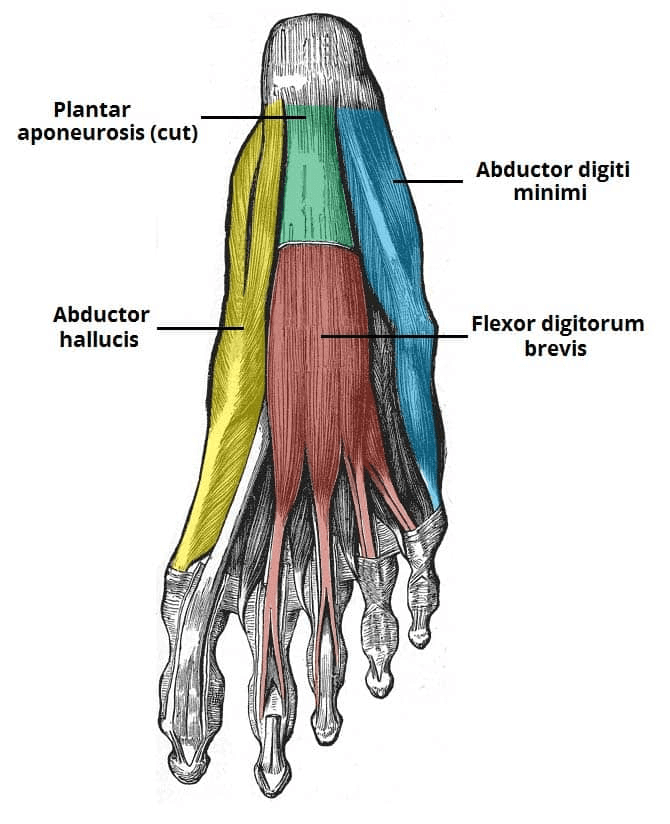
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
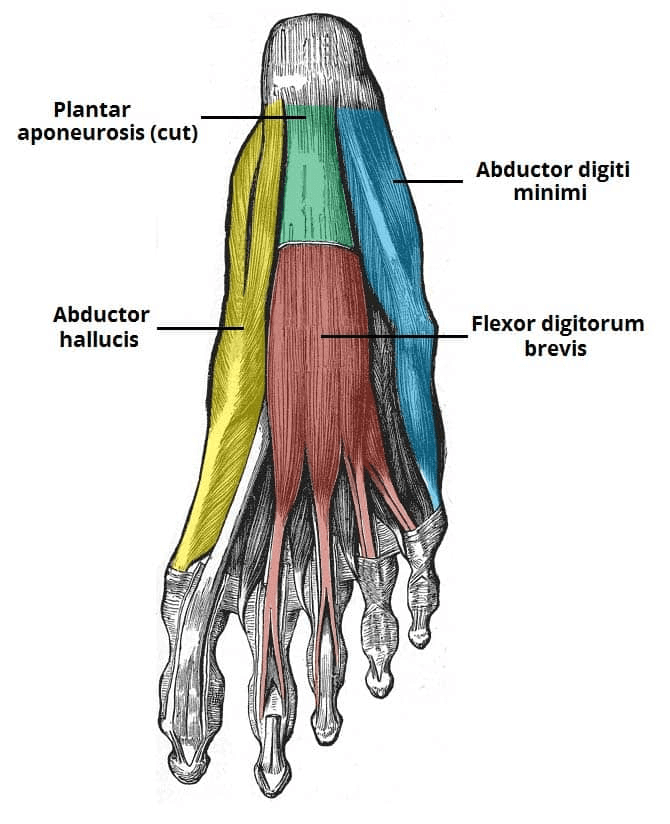
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
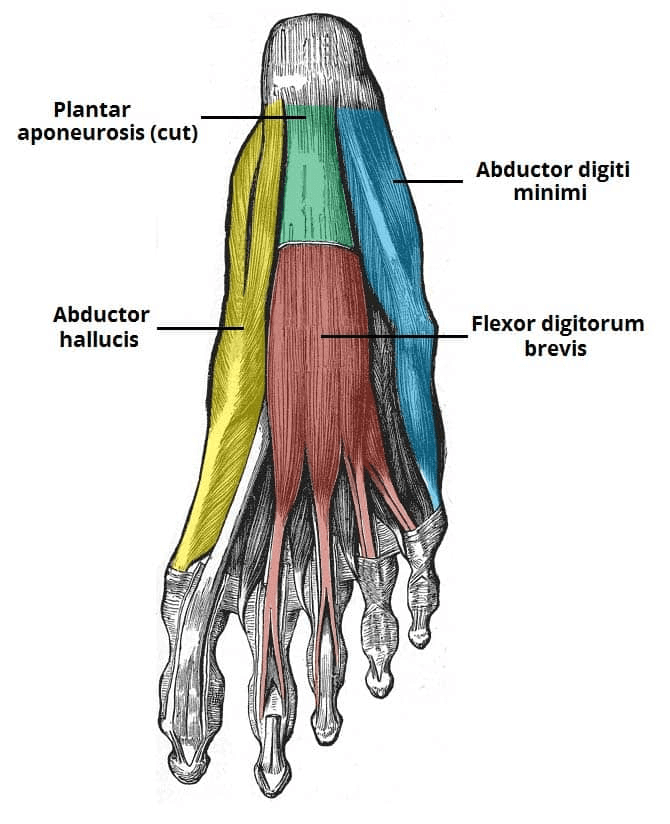
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
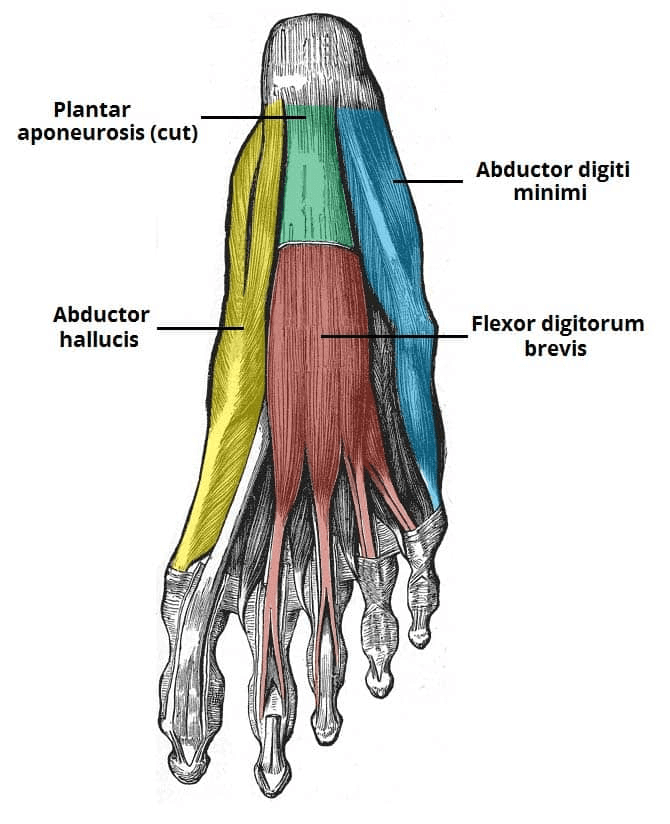
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
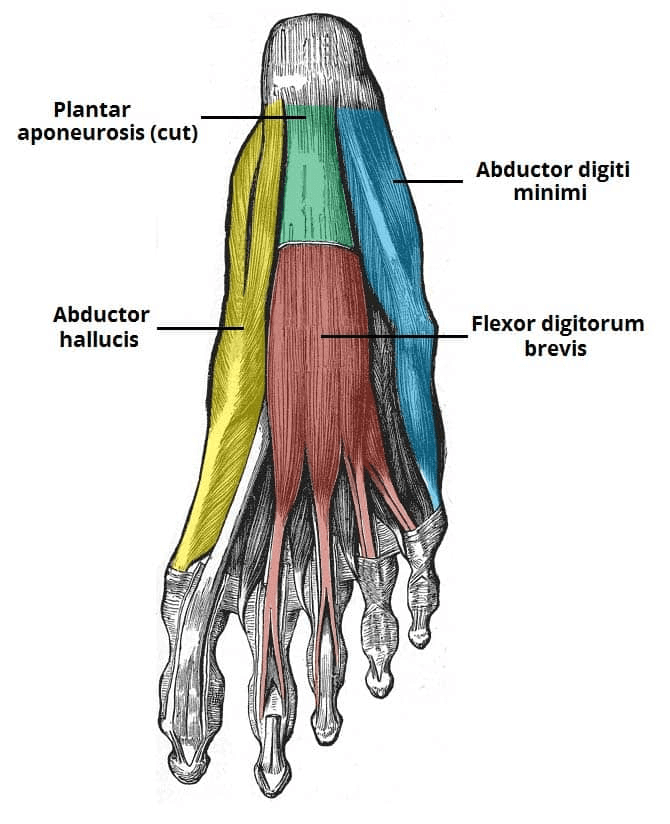
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

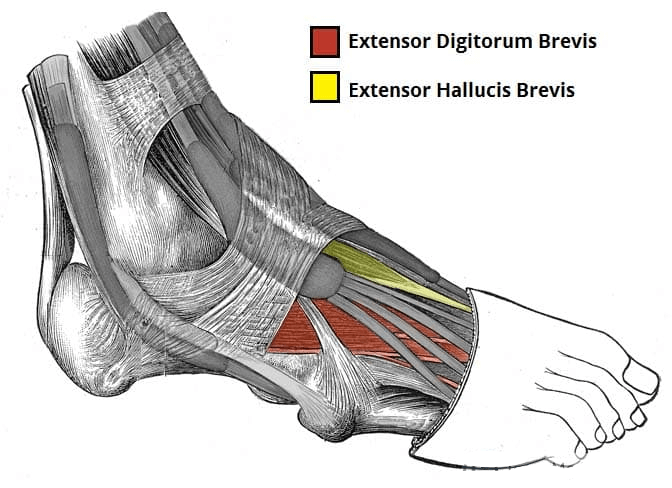
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
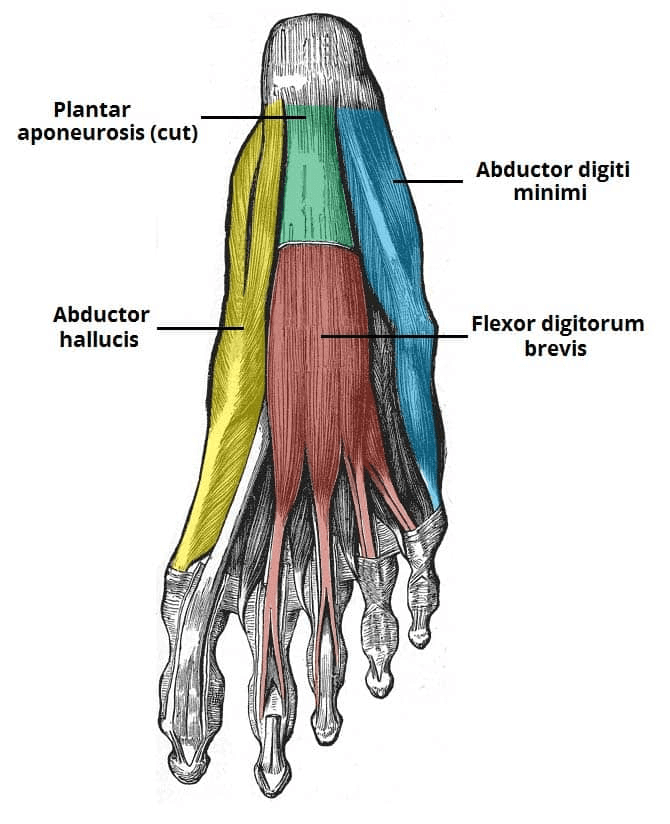
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

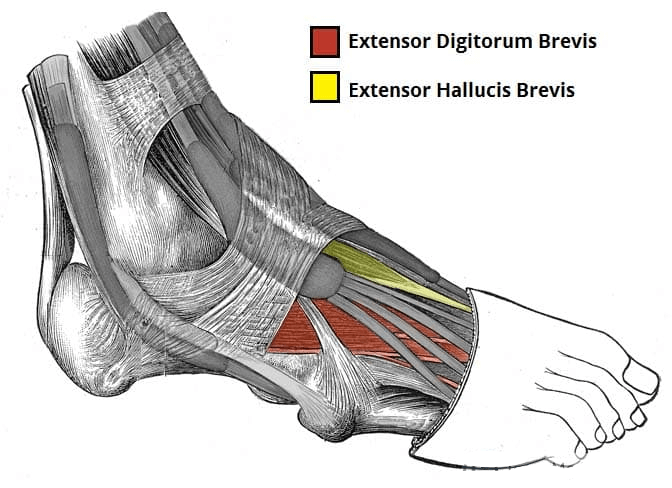
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
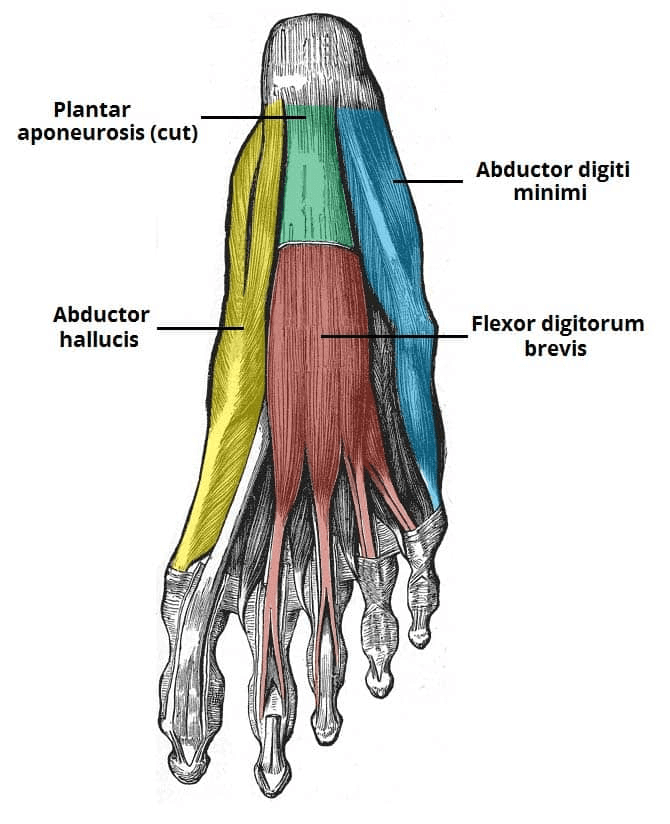
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Extensor Hallucis Brevis
The extensor hallucis brevis is often considered to be the medial part of the extensor digitorum brevis muscle, rather than a separate structure.
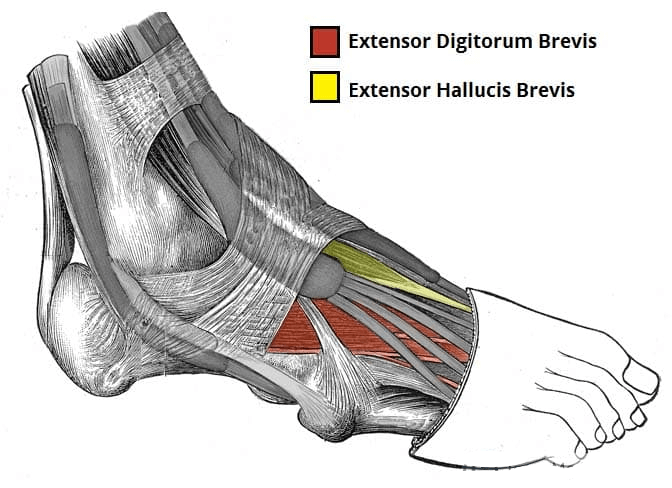
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
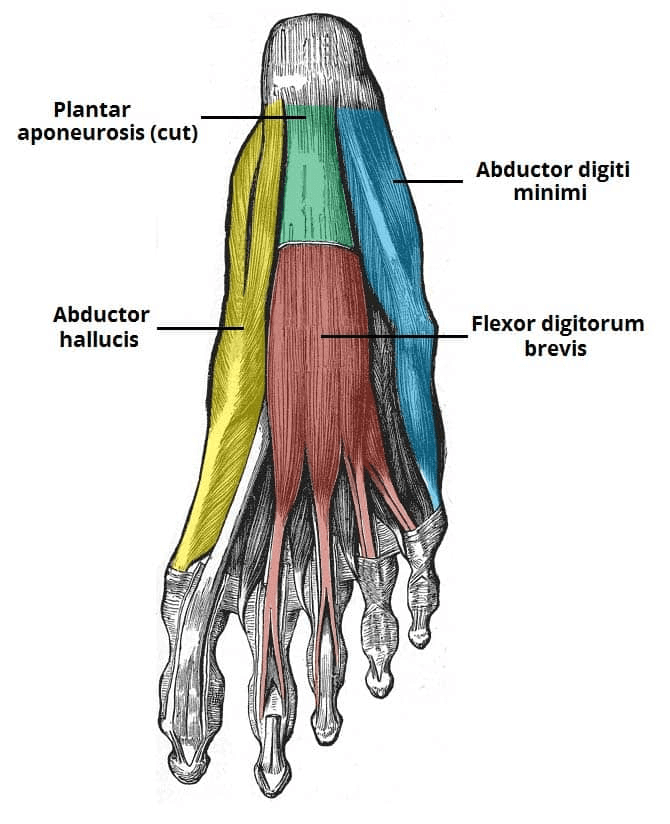
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

Extensor Hallucis Brevis
The extensor hallucis brevis is often considered to be the medial part of the extensor digitorum brevis muscle, rather than a separate structure.
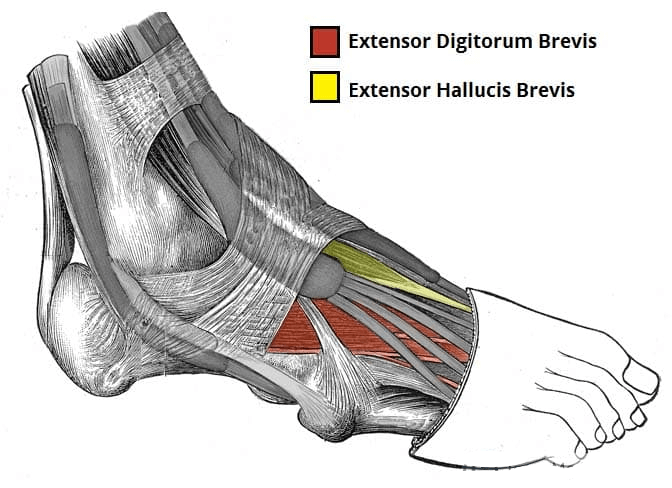
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
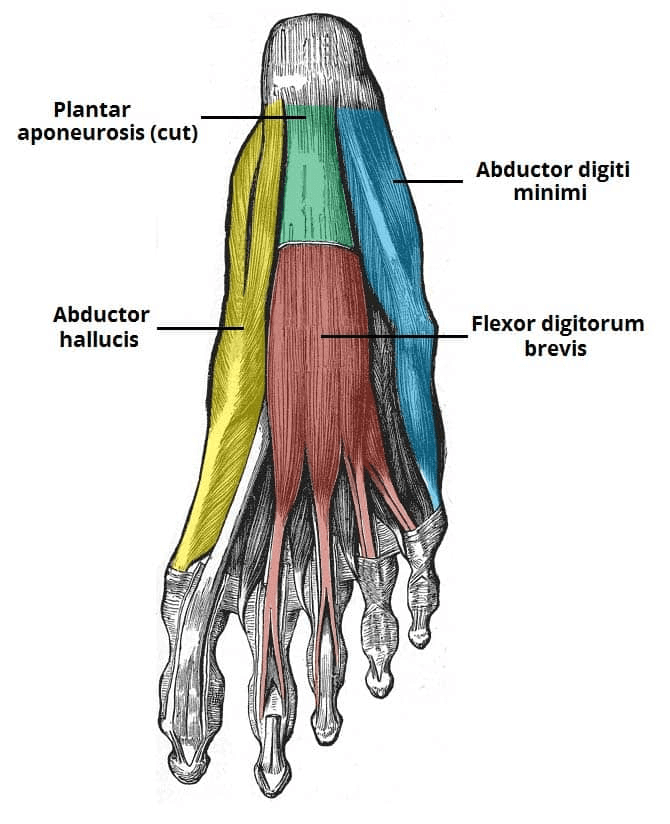
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

There are two intrinsic muscles located within the dorsum of the foot – the extensor digitorum brevis and extensor hallucis brevis.
They assist the extrinsic muscles of the foot in extending the toes and are both innervated by the deep fibular nerve.
Extensor Digitorum Brevis
The extensor digitorum brevis is a small, thin muscle which lies underneath the long extensor tendons of the foot.
Extensor Hallucis Brevis
The extensor hallucis brevis is often considered to be the medial part of the extensor digitorum brevis muscle, rather than a separate structure.
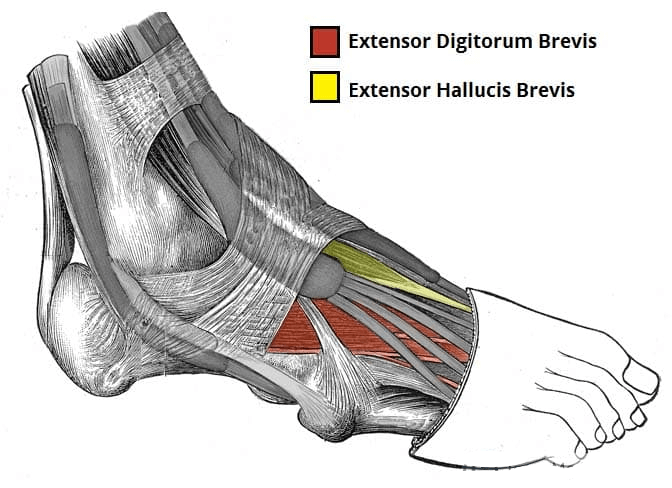
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
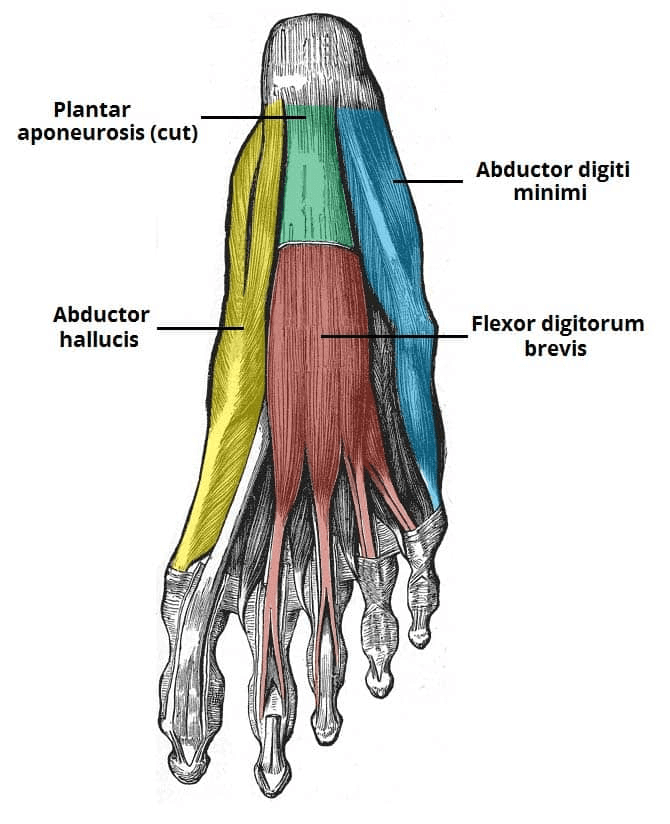
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

In this article, we shall examine the anatomy of the intrinsic muscles of the foot. They can be divided into those situated on the dorsum of the foot, and those in the sole of the foot.
There are two intrinsic muscles located within the dorsum of the foot – the extensor digitorum brevis and extensor hallucis brevis.
They assist the extrinsic muscles of the foot in extending the toes and are both innervated by the deep fibular nerve.
Extensor Digitorum Brevis
The extensor digitorum brevis is a small, thin muscle which lies underneath the long extensor tendons of the foot.
Extensor Hallucis Brevis
The extensor hallucis brevis is often considered to be the medial part of the extensor digitorum brevis muscle, rather than a separate structure.
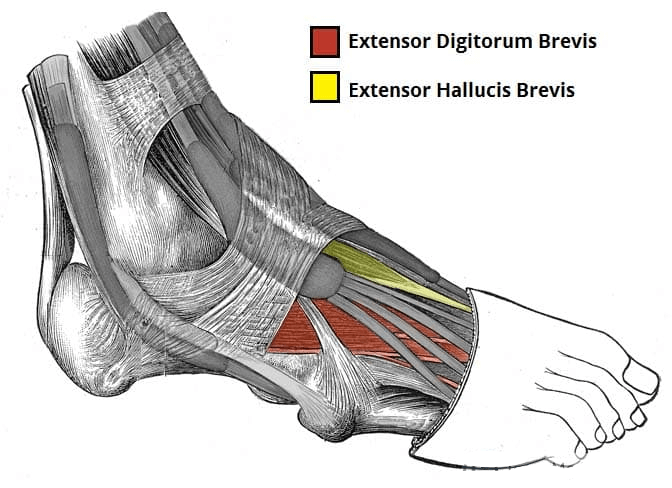
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
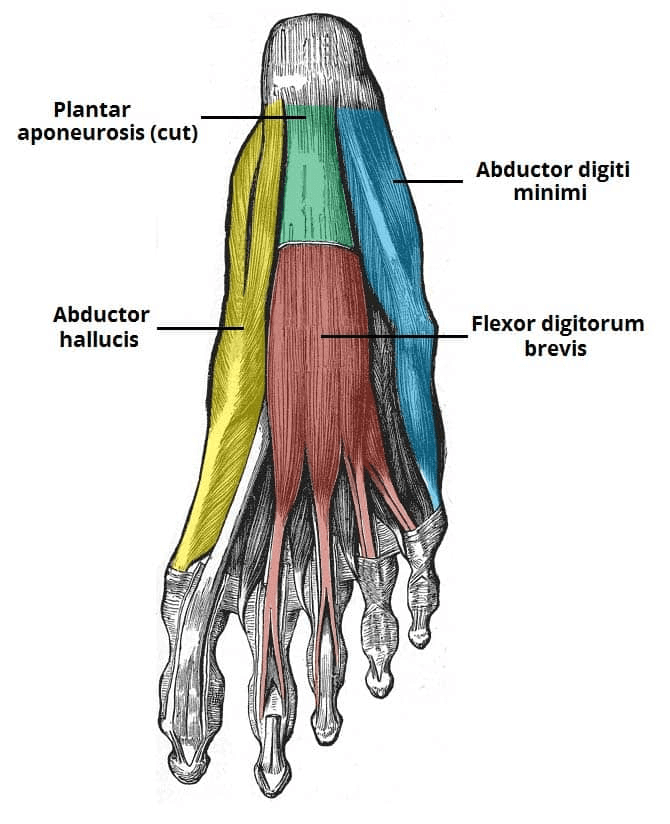
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.

In this article, we shall examine the anatomy of the intrinsic muscles of the foot. They can be divided into those situated on the dorsum of the foot, and those in the sole of the foot.
There are two intrinsic muscles located within the dorsum of the foot – the extensor digitorum brevis and extensor hallucis brevis.
They assist the extrinsic muscles of the foot in extending the toes and are both innervated by the deep fibular nerve.
Extensor Digitorum Brevis
The extensor digitorum brevis is a small, thin muscle which lies underneath the long extensor tendons of the foot.
Extensor Hallucis Brevis
The extensor hallucis brevis is often considered to be the medial part of the extensor digitorum brevis muscle, rather than a separate structure.
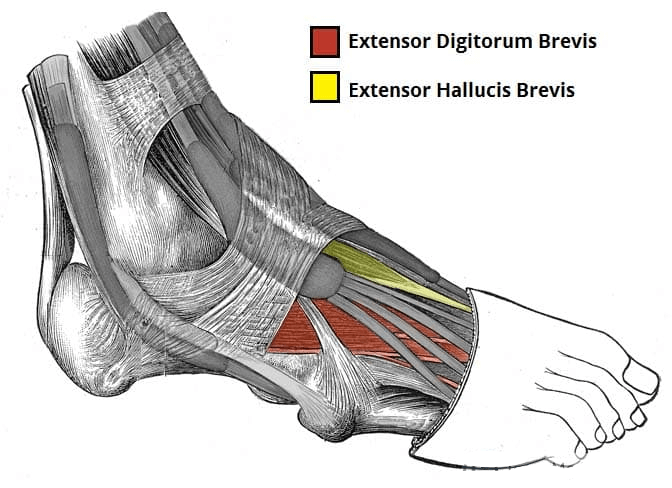
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
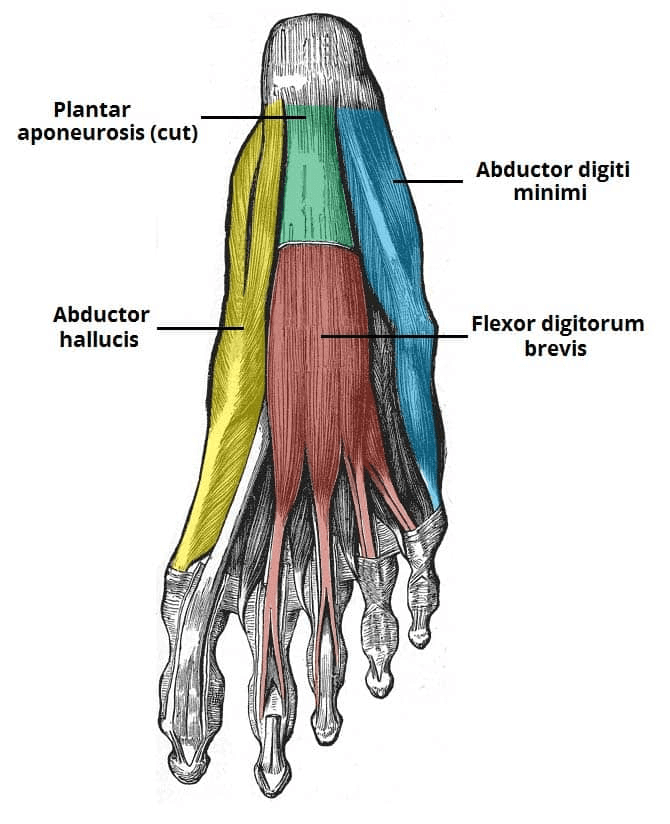
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


The muscles acting on the foot can be divided into two distinct groups; extrinsic and intrinsic muscles.
In this article, we shall examine the anatomy of the intrinsic muscles of the foot. They can be divided into those situated on the dorsum of the foot, and those in the sole of the foot.
There are two intrinsic muscles located within the dorsum of the foot – the extensor digitorum brevis and extensor hallucis brevis.
They assist the extrinsic muscles of the foot in extending the toes and are both innervated by the deep fibular nerve.
Extensor Digitorum Brevis
The extensor digitorum brevis is a small, thin muscle which lies underneath the long extensor tendons of the foot.
Extensor Hallucis Brevis
The extensor hallucis brevis is often considered to be the medial part of the extensor digitorum brevis muscle, rather than a separate structure.
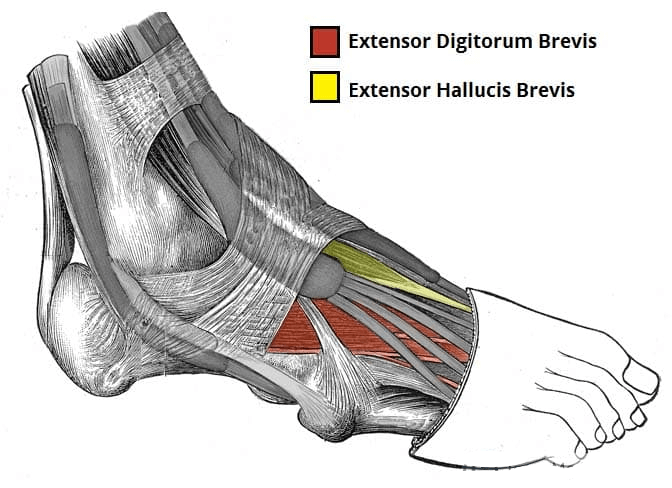
There are ten intrinsic muscles located in the plantar aspect (sole) of the foot.
They act collectively to stabilise the arches of the foot and individually to control movement of the digits. They are innervated by the medial or lateral plantar nerves – which are branches of the tibial nerve.
The muscles of the plantar aspect are arranged in four layers (superficial to deep):
First Layer
The first layer contains three muscles. It is the most superficial and is located immediately underneath the plantar fascia.
Abductor Hallucis
The abductor hallucis muscle is located on the medial side of the sole, where it contributes to a small soft tissue bulge.
Flexor Digitorum Brevis
The flexor digitorum brevis muscle is located laterally to the abductor hallucis. It sits in the centre of the sole, sandwiched between the plantar aponeurosis and the tendons of flexor digitorum longus.
Abductor Digiti Minimi
The abductor digiti minimi muscle is located on the lateral side of the foot. It is homologous with the abductor digiti minimi of the hand.
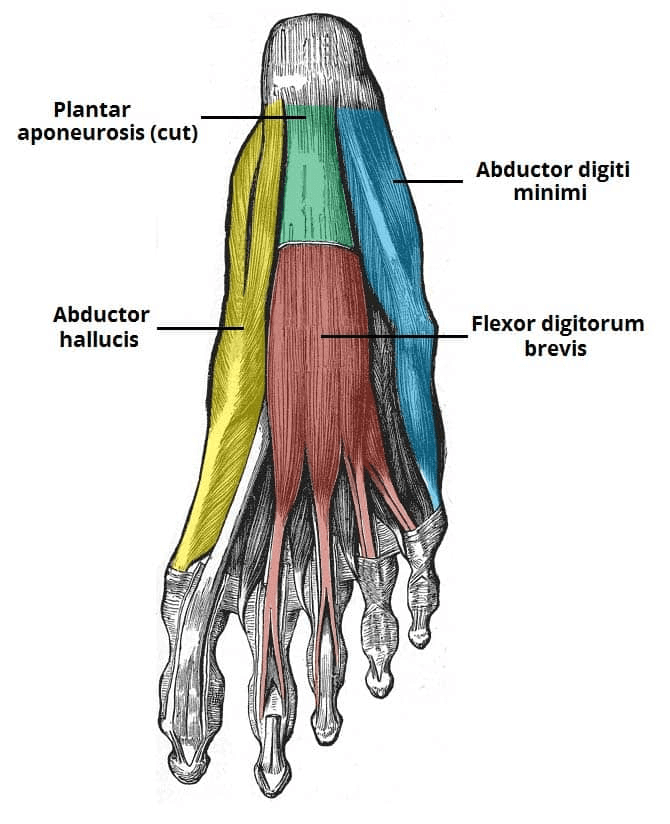
Second Layer
The second plantar layer contains two muscles – the quadratus plantae and the lumbricals. The tendons of the flexor digitorum longus (an extrinsic muscle) also travel through this layer.
Quadratus Plantae
The quadratus plantae is a flat, square-shaped muscle with two heads of origin.
Lumbricals
There are four lumbrical muscles in the foot. They are each located medial to their respective tendon of the flexor digitorum longus.

Third Layer
The third layer contains three muscles. The flexor hallucis brevis and adductor hallucis are associated with movements of the great toe. The remaining muscle, the flexor digiti minimi brevis, moves the little toe.
Flexor Hallucis Brevis
The flexor hallucis brevis muscle is located on the medial side of the foot. It has two heads of origin.
Adductor Hallucis
The adductor hallucis muscle is located laterally to the flexor hallucis brevis. It consists of an oblique and transverse head.
Flexor Digiti Minimi Brevis
The flexor digiti minimi brevis muscle is located on the lateral side of the foot, underneath the metatarsal of the little toe. It resembles the interossei in structure.

Fourth Later
The plantar and dorsal interossei comprise the fourth and final plantar muscle layer. The plantar interossei have a unipennate shape, while the dorsal interossei are bipennate.
Plantar Interossei
There are three plantar interossei, which are located between the metatarsals. Each arises from a single metatarsal.
Dorsal Interossei
There are four dorsal interossei, which are located between the metatarsals. Each arises from two metatarsals.


Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.
Tendinopathy, which is a chronic degenerative condition is not associated with an inflammatory response.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.

Tendinopathy, which is a chronic degenerative condition is not associated with an inflammatory response.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.
The endurance trained tendons are capable of storing elastic energy very well over longer periods of time. The sprint trained tendons are capable of storing and releasing a high amount of tension for very short periods of time.
Like any other system in the body, tendons need rest to recover and adapt to stress.
Acute tendon injuries may be caused by a single traumatic event. However, chronic overuse is often the catalyst to the singular event.
Tendon related injuries are often categorized into two types. Tendinitis, which suggests a pro inflammatory environment. This tends to last 1-2 weeks and will often resolve if the stimulus is removed.

Tendinopathy, which is a chronic degenerative condition is not associated with an inflammatory response.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.
Training programs can vary in frequency, intensity, time and type. If we consider a spectrum of training exposure at the extremes- endurance activity like marathons, or high intensity sprints, we can then see specific adaptations to the demands of that training.
Endurance type exercise tends to result in thinner and longer tendons. Sprinting type exercises tend to result in thicker and shorter tendons.
The endurance trained tendons are capable of storing elastic energy very well over longer periods of time. The sprint trained tendons are capable of storing and releasing a high amount of tension for very short periods of time.
Like any other system in the body, tendons need rest to recover and adapt to stress.
Acute tendon injuries may be caused by a single traumatic event. However, chronic overuse is often the catalyst to the singular event.
Tendon related injuries are often categorized into two types. Tendinitis, which suggests a pro inflammatory environment. This tends to last 1-2 weeks and will often resolve if the stimulus is removed.

Tendinopathy, which is a chronic degenerative condition is not associated with an inflammatory response.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.
Tendons are made up of collagen fibrils that wrap around each other to create progressively thicker bundles that are then wrapped in sheaths. This specific scaffolding structure creates resiliency by allowing the bands to create tension at varying degrees of intensity.
Training programs can vary in frequency, intensity, time and type. If we consider a spectrum of training exposure at the extremes- endurance activity like marathons, or high intensity sprints, we can then see specific adaptations to the demands of that training.
Endurance type exercise tends to result in thinner and longer tendons. Sprinting type exercises tend to result in thicker and shorter tendons.
The endurance trained tendons are capable of storing elastic energy very well over longer periods of time. The sprint trained tendons are capable of storing and releasing a high amount of tension for very short periods of time.
Like any other system in the body, tendons need rest to recover and adapt to stress.
Acute tendon injuries may be caused by a single traumatic event. However, chronic overuse is often the catalyst to the singular event.
Tendon related injuries are often categorized into two types. Tendinitis, which suggests a pro inflammatory environment. This tends to last 1-2 weeks and will often resolve if the stimulus is removed.

Tendinopathy, which is a chronic degenerative condition is not associated with an inflammatory response.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.

The tendon is an elastic tissue that anchors muscles to bones. Tendons receive their nutrition from movement (tension created by muscle), rather than blood, like muscles. Similar to muscles, tendons can improve their strength. The type of stress (exercise) tendons are exposed to will determine their functional capacity.
Tendons are made up of collagen fibrils that wrap around each other to create progressively thicker bundles that are then wrapped in sheaths. This specific scaffolding structure creates resiliency by allowing the bands to create tension at varying degrees of intensity.
Training programs can vary in frequency, intensity, time and type. If we consider a spectrum of training exposure at the extremes- endurance activity like marathons, or high intensity sprints, we can then see specific adaptations to the demands of that training.
Endurance type exercise tends to result in thinner and longer tendons. Sprinting type exercises tend to result in thicker and shorter tendons.
The endurance trained tendons are capable of storing elastic energy very well over longer periods of time. The sprint trained tendons are capable of storing and releasing a high amount of tension for very short periods of time.
Like any other system in the body, tendons need rest to recover and adapt to stress.
Acute tendon injuries may be caused by a single traumatic event. However, chronic overuse is often the catalyst to the singular event.
Tendon related injuries are often categorized into two types. Tendinitis, which suggests a pro inflammatory environment. This tends to last 1-2 weeks and will often resolve if the stimulus is removed.

Tendinopathy, which is a chronic degenerative condition is not associated with an inflammatory response.
General treatment approached for tendon related pathologies include refraining from symptom provoking activity, reducing training workload, continue to strength train non-symptom provoking muscle groups.
Tendon specific training after a tendon related injury may initially include isometrics and eccentrics.
Isometrics (creating muscle tension without joint movement) may allow the muscle-tendon unit to maintain healthy function without provoking symptoms, resulting in persistent inflammation or further degeneration of the tendon.

Eccentrics is loading the muscle tendon unit in the lengthening phase only. It has similar benefits as isometric loading. In addition, you may load the tendon up to 2.5x more than if you were performing the entire cycle itself- concentric, then eccentric. In this way, we can create a tendon that is capable of withstanding more than what the concentric only portion of a lift can handle. However, this high of a load may not be feasible for all tendons at all times.

Outside of treating tendon injuries, plyometric exercises and time under tension are two sport specific ways to improve tendon strength and resiliency. As stated above, plyometric exercises including sprinting result in thicker tendons. Time under tension including long distance running result in longer and more elastic tendons.
Generally speaking, one does not have to ‘create’ additional tendon strengthening programs as the program designed for a specific muscle function is often adequate enough. You do not need to do additional “sprints for tendons” since the sprinting itself is a program for tendon, muscular and cardiovascular fitness in and of itself.
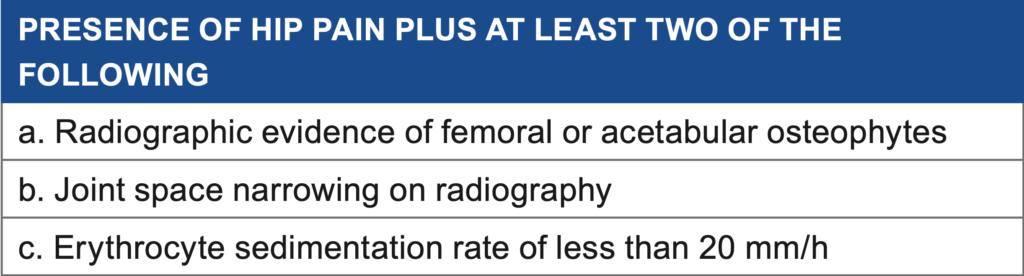
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
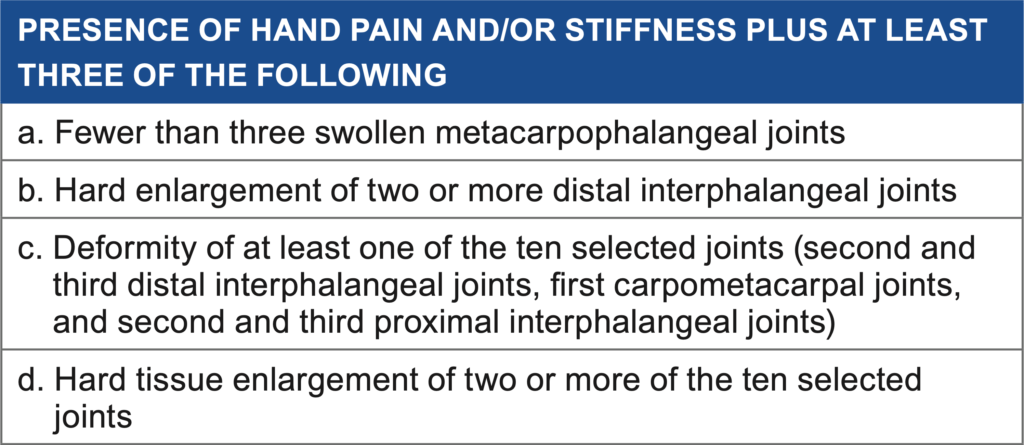
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
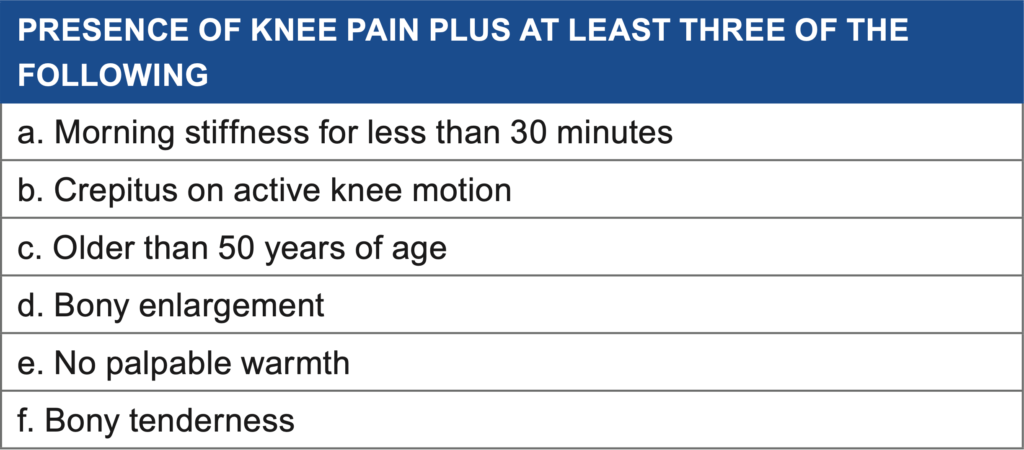
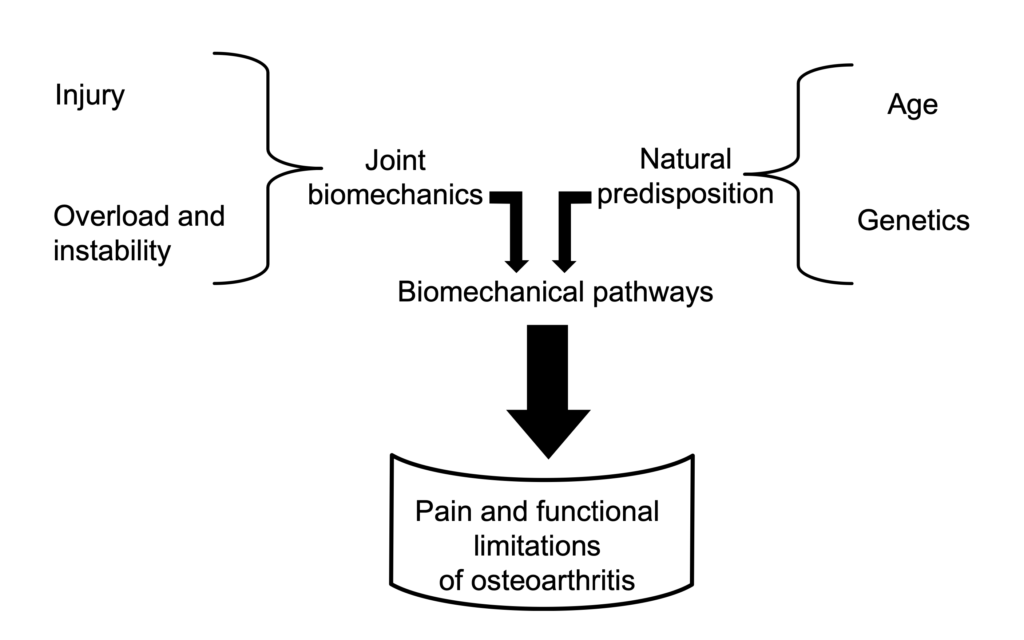
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
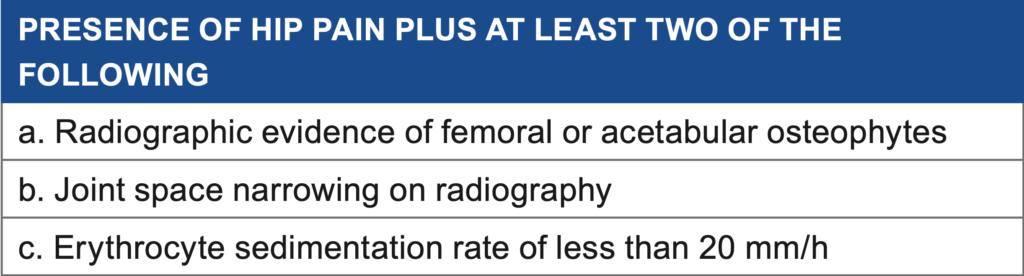
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
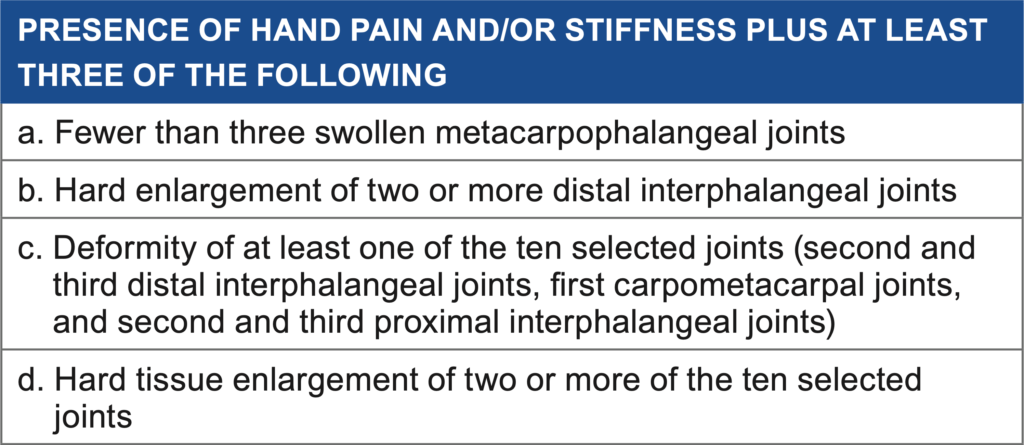
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
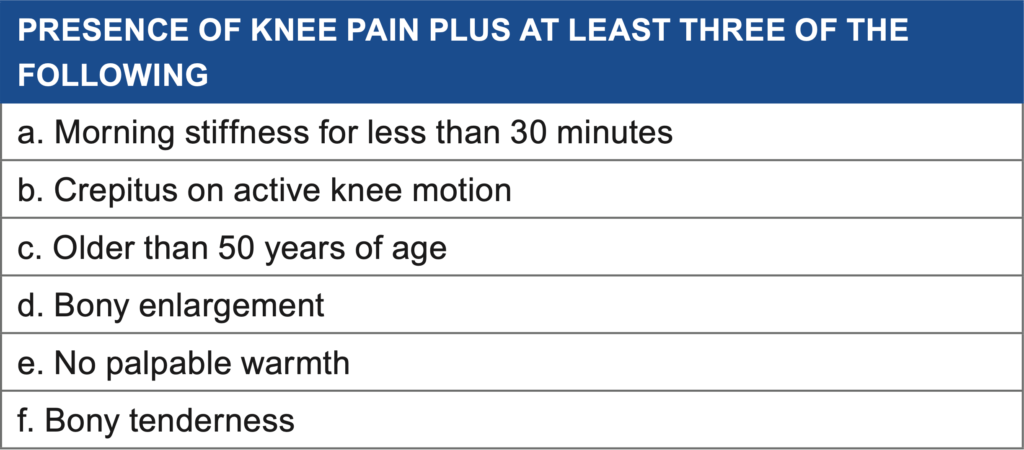
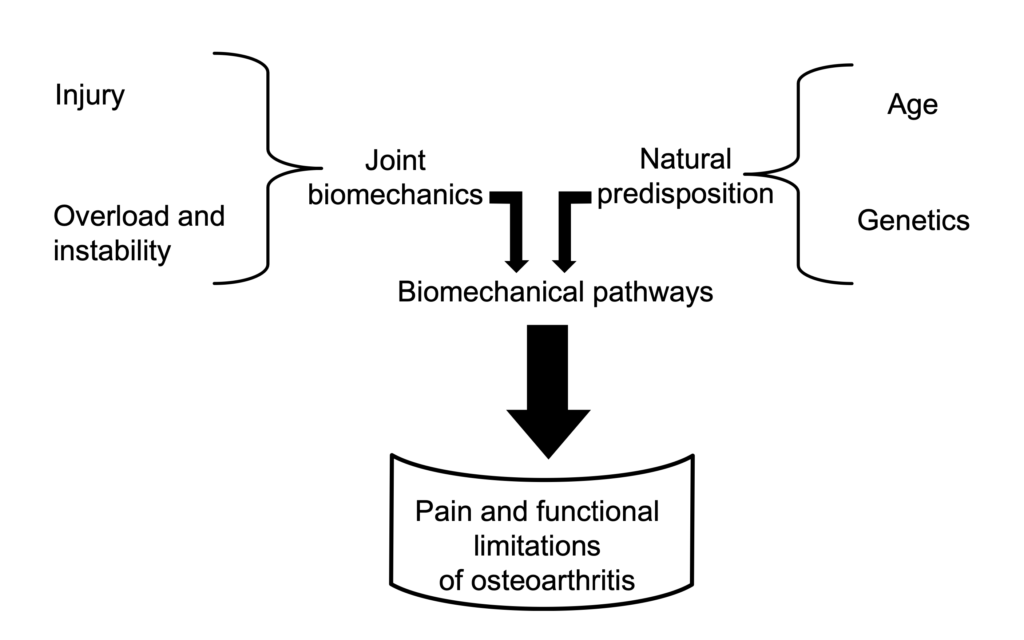
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
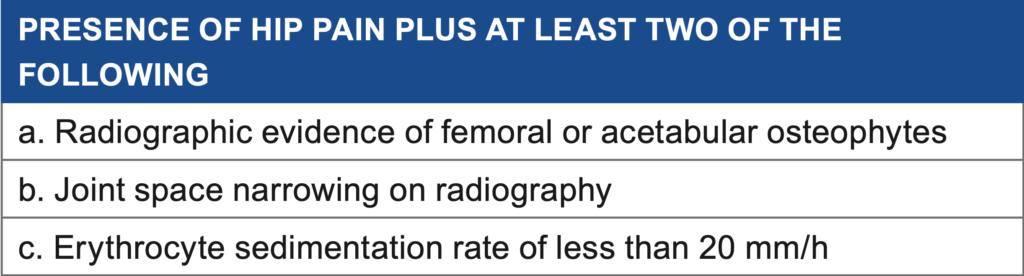
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
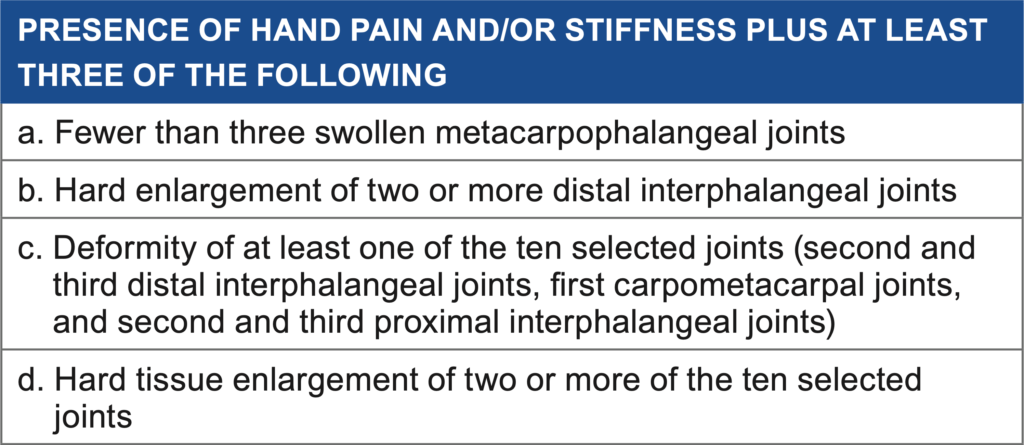
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
Sports that cause direct trauma to joints, including football, soccer, lacrosse and rugby, account for most of the traumatic onset. About 80% of former football players developed OA 10-30 years after competing. One component of the athletic endeavor includes a higher rate of loading and frequency, disrupting cartilage repair.
Cartilage is designed to withstand compressive forces. However, if inadequate time is allowed for the tissue to rest, the surface may become damaged, exposing sensitive tissue underneath.
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
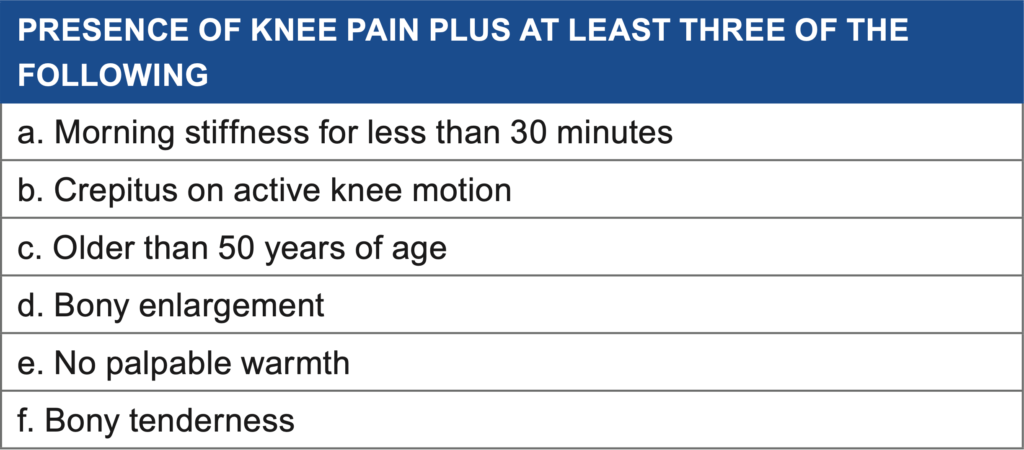
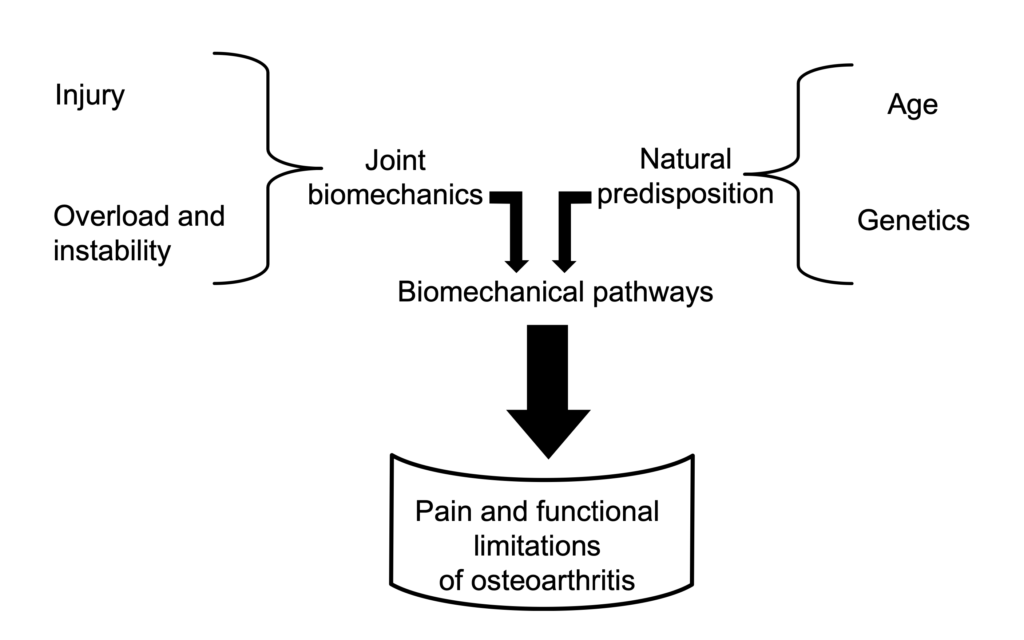
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
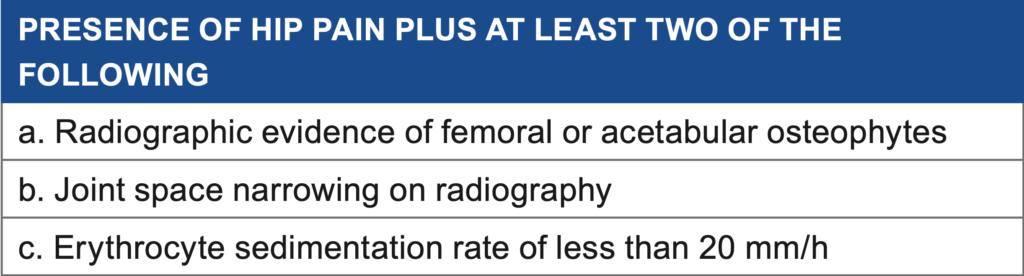
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
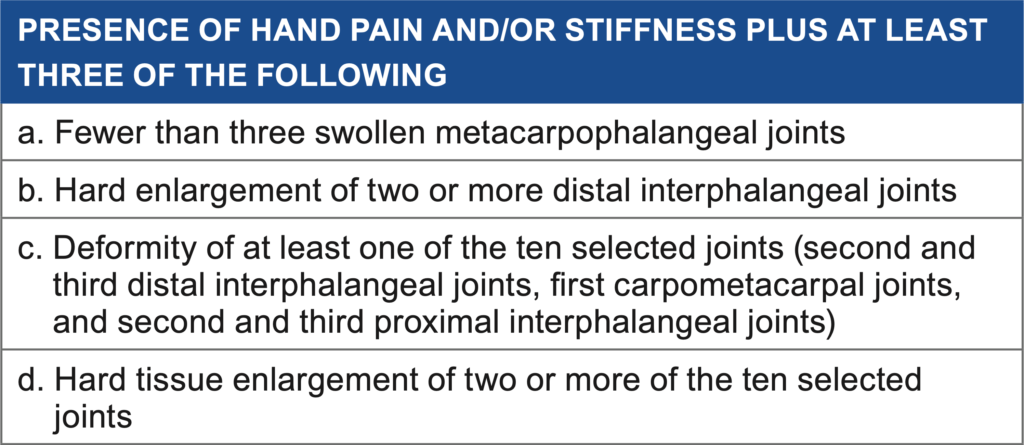
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
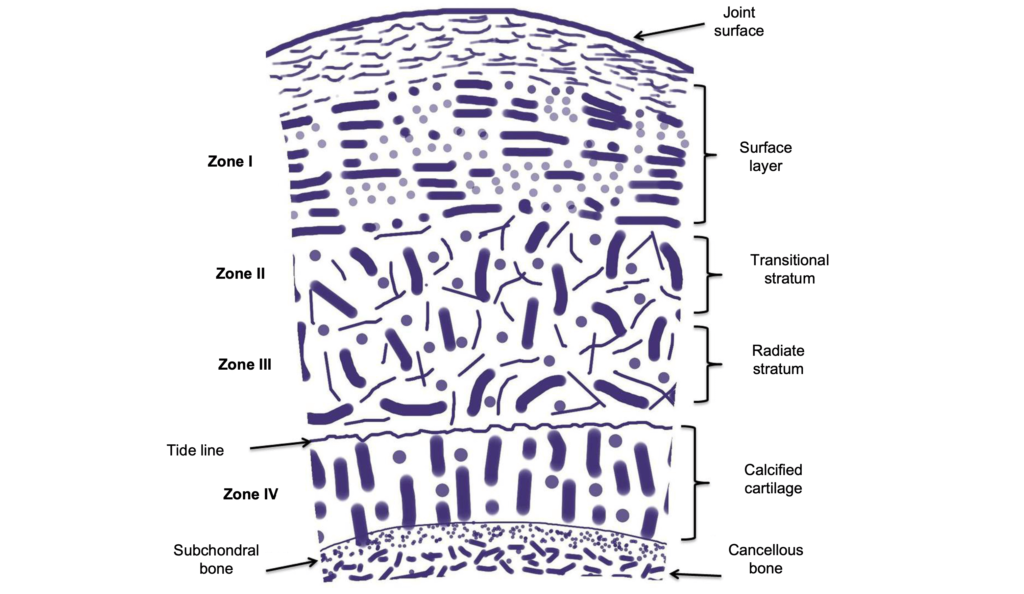
Genetics, obesity, joint injury, occupation, gender and race are risk factors for the onset and progression of OA.
Sports that cause direct trauma to joints, including football, soccer, lacrosse and rugby, account for most of the traumatic onset. About 80% of former football players developed OA 10-30 years after competing. One component of the athletic endeavor includes a higher rate of loading and frequency, disrupting cartilage repair.
Cartilage is designed to withstand compressive forces. However, if inadequate time is allowed for the tissue to rest, the surface may become damaged, exposing sensitive tissue underneath.
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
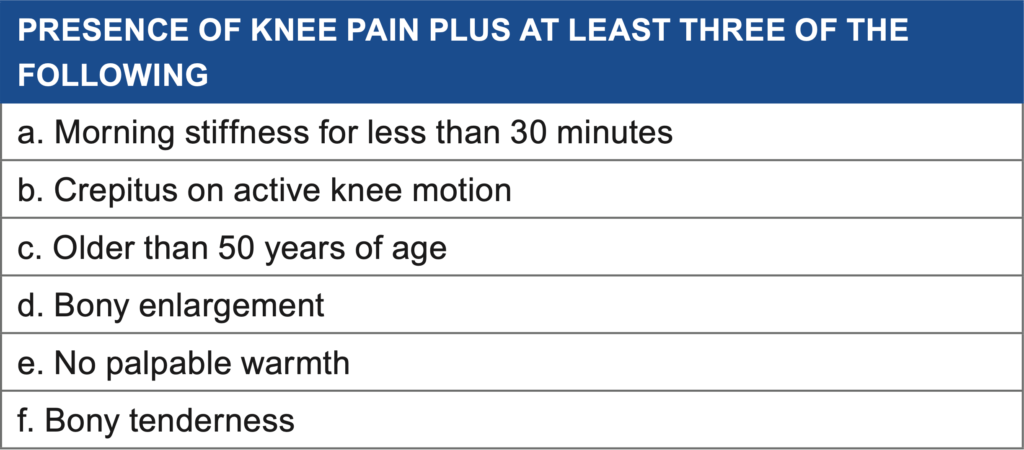
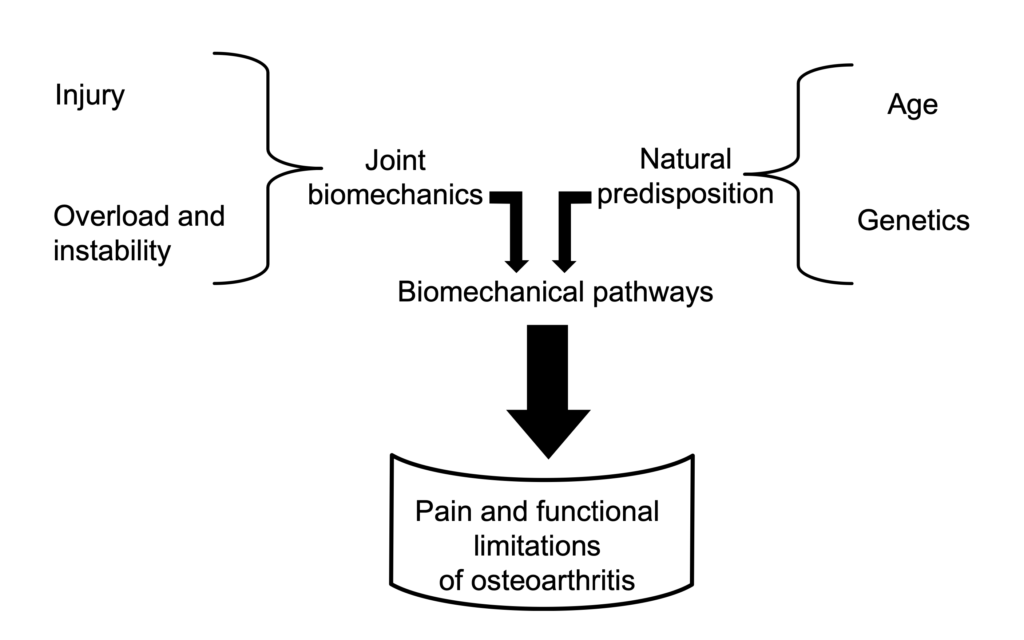
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
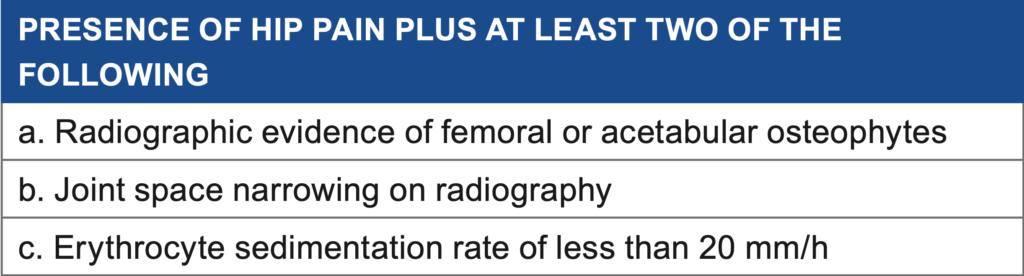
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
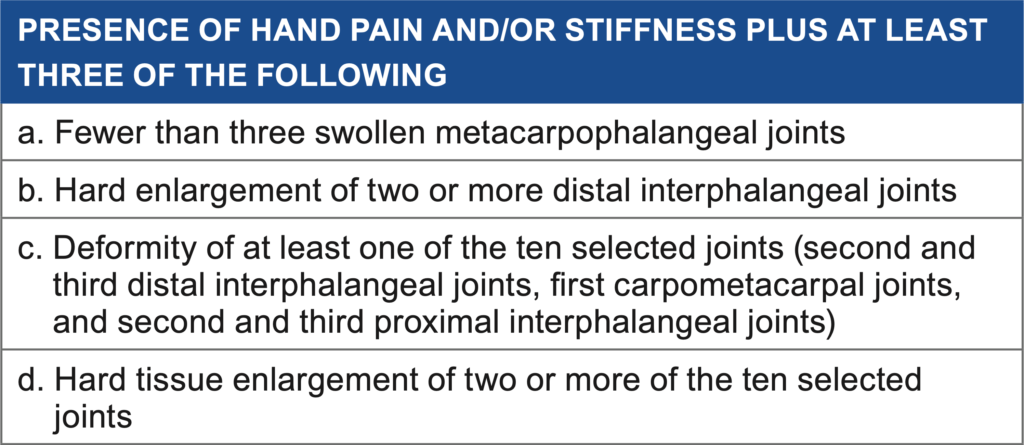
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.

Osteoarthritis (OA) is caused by a defect in the joint cartilage. Cartilage is a soft, spongy type of tissue, well lubricated, designed to minimize friction between two surfaces. As we age, the cartilage becomes less lubricated, wearing out the more superficial layers, resulting in pain & dysfunction.
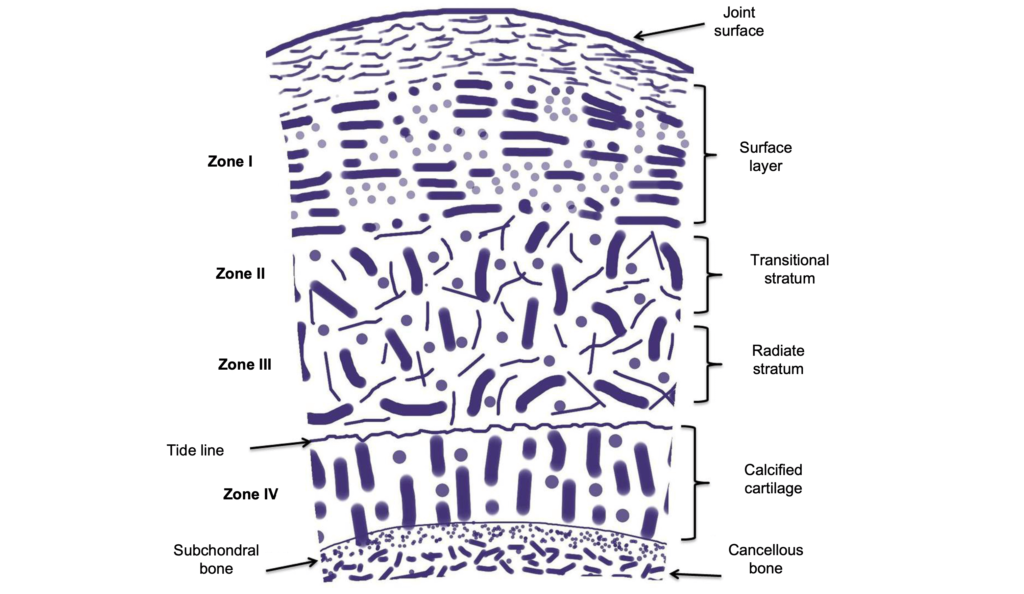
Genetics, obesity, joint injury, occupation, gender and race are risk factors for the onset and progression of OA.
Sports that cause direct trauma to joints, including football, soccer, lacrosse and rugby, account for most of the traumatic onset. About 80% of former football players developed OA 10-30 years after competing. One component of the athletic endeavor includes a higher rate of loading and frequency, disrupting cartilage repair.
Cartilage is designed to withstand compressive forces. However, if inadequate time is allowed for the tissue to rest, the surface may become damaged, exposing sensitive tissue underneath.
Chronic injury of the cartilage is often described as stiff, aching upon waking. The symptoms generally start as discomfort and is relieved with movement, usually after 30 or so minutes. As the condition progresses, joint grinding and cracking may be noted. This eventually leads to less use of the limb, resulting in muscle atrophy and further joint restrictions.
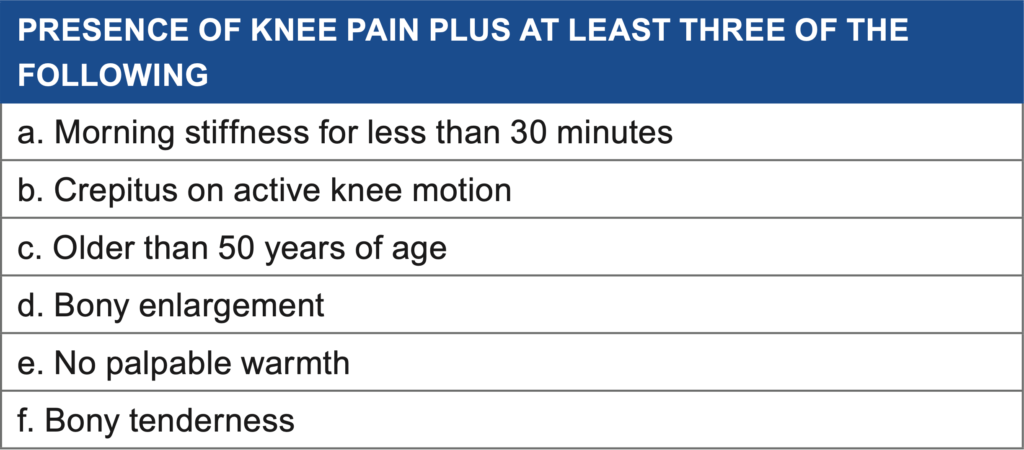
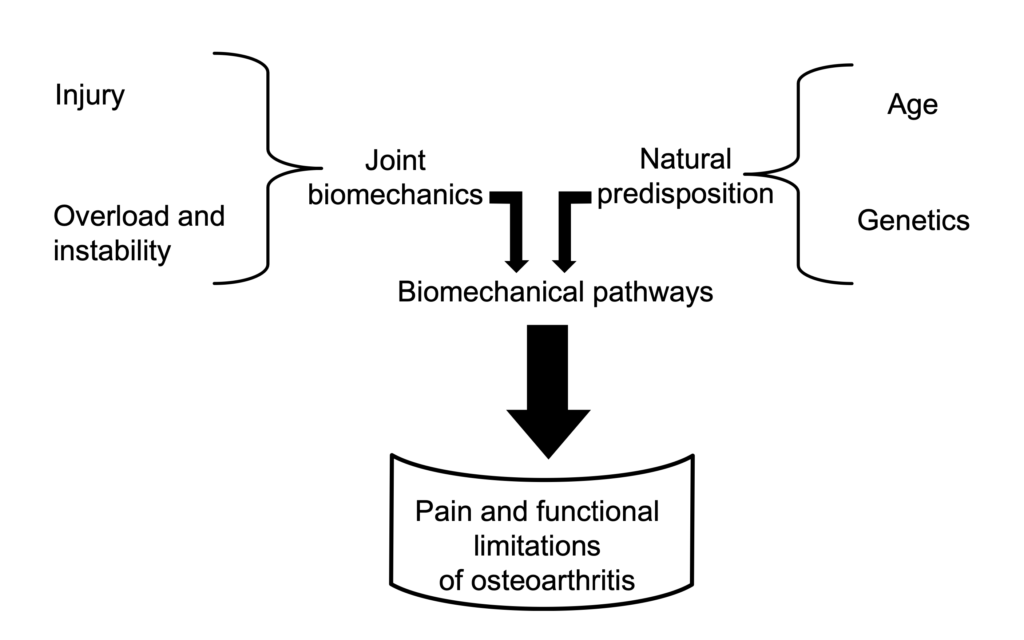
Radiographs (x-rays) can be taken to diagnose extent and location of the cartilage damage. However, there is little correlation between the grading of OA and the pain and individual may experience. X-rays can also visualize osteophytes, joint space narrowing, subchondral sclerosis and cysts.
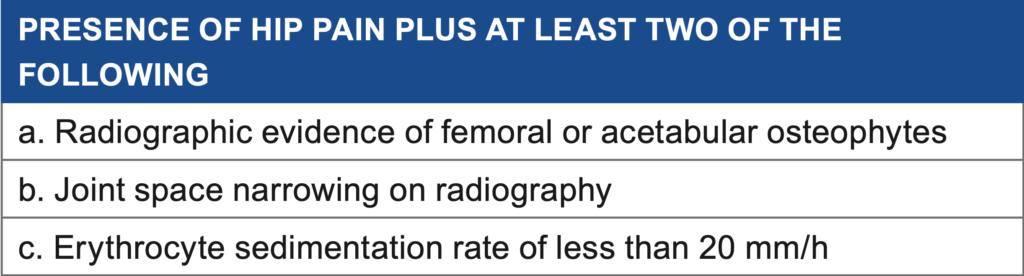
Treatment for OA focuses mainly on exercises to improve muscle strength, joint mobility, and flexibility. Over the counter pain medication may be useful during flare ups. Exercise can be modified to accomodate dysfunction, experience with equipment and pain.
Other treatment may include hyaluronic acid which has anti-inflammatory and analgesic effects. If the disease progresses to a point where the individual is dysfunctional and has not favorably responded to conservative treatment (physical therapy, medication, injections), then a joint replacement may be recommended.
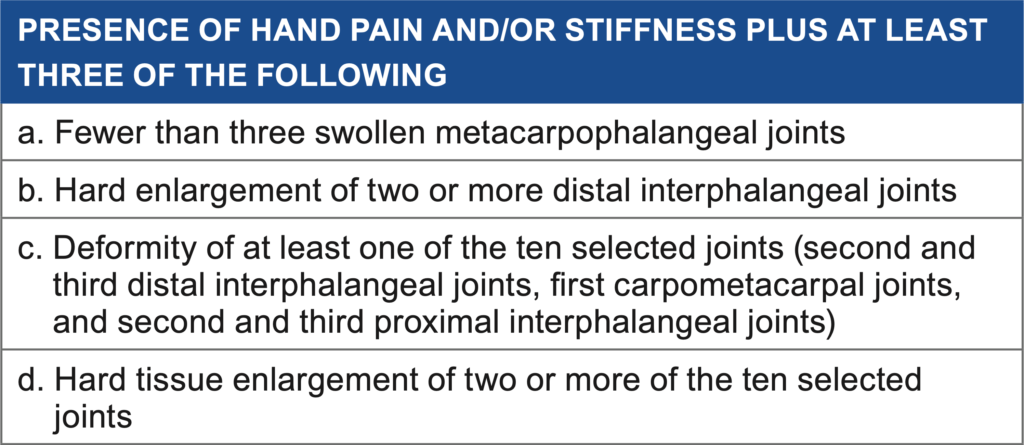
The few studies that have investigated total knee replacement in younger patients ( 50 years ) have shown successful rates after an average follow-up of eight years.
Typical shoulder injuries might appear low grade at first and then rapidly deteriorate if not treated in due time. Pinching in the front of the shoulder when reaching overhead or across the chest might suggest supraspinatus (rotator cuff) impingement. The muscle is “wrung out” between two bones- the AC joint and the head of the humerus, the attachment site for the muscle. This constant pinching causes fraying of the tendon, leading to tiny tears. The body then begins to deposit fat in these tears to stabilize the area. As you might guess, fat does not do as good a job as the original tendon for transferring force from the muscle into the shoulder to produce movement (like pushing your opponent to set them up). This small tearing reduces the work capacity of the muscle and other muscles must compensate for poor movement patterns.
Neck injuries can vary from muscle aches (getting out of bed in the morning, but relief after moving around) that can be treated without any significant loss of training to severe neurological compromise requiring surgery (numbness, tingling or significant weakness of the arms or legs). Most often injuries involving the muscles can limit your ability to look around, may feel “stiff” when waking up and cause pain with certain movements, like slipping a punch. Muscular strains are often treated with hands on techniques and muscle re-education program. More serious injuries may require consultation with an orthopedic or sports medicine physician.
Combat sport athletes should be cautious of and take care of injuries in the lower back. Most back pain injuries involve soft tissue- tendons, muscles and ligaments. Fractures, herniated discs and degenerative disc disease in more seasoned athletes are typical. These injuries can present in many different ways. Some may have pain with movement, others may have relief with movement in certain directions. The pain might feel better with standing or worse with sitting. It is important to accurately identify what structure might be causing pain and to treat it accordingly
Grappling requires a balance between very flexible, but strong hips. In the guard your hips are in flexion, abduction and relative external rotation. As your opponent is passing the guard, they may force your knee across your chest into your opposite shoulder (ex. right knee, left shoulder). This compresses the hip labrum, a soft, pliable tissue like rubber. If the labrum is torn it can cause a sharp pinching pain when you are caught in this position.
Ankle sprains occur when the foot is rolled under the body, tearing the ligament that connects the ankle to the foot. Lunging and squatting may cause this area to “pinch”. Ankle sprains typically cause the feeling of “giving way” when working your stand up game, or occasional misplacing of the foot because your brains processing of where your body is in space is disrupted.
Pain along the outside of the elbow, right on top of the radial head where the muscle mass attaches into, is called lateral epicondylagia (formerly known as epicondylitis). With tendon damage, the inflammatory phase lasts about a week and thereafter the tissue begins to heal (now no longer an “-itis”). In some injuries the tissue being laid down to replace the torn tendon is not as strong. This can lead to fraying of the tendon and fatty deposits in an attempt to stabilize the area. The fraying reduces the total amount of strength the tendon can handle. The fatty deposits alter the proper line of pull when the muscle contracts. All this being said, when you go to grab your opponents gi, wrist or leg to control it, pain hits and suddenly you cant squeeze as hard.
If you want the extended version with tips on how to prevent these injuries download The Ultimate Guide to Major MMA Injuries by Dr. Abbate.
Dr. Abbate has committed his professional career to studying all aspects of combat sports with a focus in injury prevention and rehabilitation. His broad knowledge in nutrition, strength and conditioning and psychology provides a strong foundation for athletes to refer to for support. If you are a coach or athlete in Miami, Florida and are concerned about an injury you may have sustained, Dr. Abbate is eager to provide support and care to keep you in the cage or on the mat.
The hand is an incredibly complex network of 29 joints, 126 ligaments, 34 tendons and their muscles, 29 bones & thick ligament-like fascia. This network allows for the manipulation of really small objects, like threading the eye of a needle, to larger objects and large movement patterns like grabbing the gi of your opponent to control them. Here is a short list of hand injuries that I often see:
Typical shoulder injuries might appear low grade at first and then rapidly deteriorate if not treated in due time. Pinching in the front of the shoulder when reaching overhead or across the chest might suggest supraspinatus (rotator cuff) impingement. The muscle is “wrung out” between two bones- the AC joint and the head of the humerus, the attachment site for the muscle. This constant pinching causes fraying of the tendon, leading to tiny tears. The body then begins to deposit fat in these tears to stabilize the area. As you might guess, fat does not do as good a job as the original tendon for transferring force from the muscle into the shoulder to produce movement (like pushing your opponent to set them up). This small tearing reduces the work capacity of the muscle and other muscles must compensate for poor movement patterns.
Neck injuries can vary from muscle aches (getting out of bed in the morning, but relief after moving around) that can be treated without any significant loss of training to severe neurological compromise requiring surgery (numbness, tingling or significant weakness of the arms or legs). Most often injuries involving the muscles can limit your ability to look around, may feel “stiff” when waking up and cause pain with certain movements, like slipping a punch. Muscular strains are often treated with hands on techniques and muscle re-education program. More serious injuries may require consultation with an orthopedic or sports medicine physician.
Combat sport athletes should be cautious of and take care of injuries in the lower back. Most back pain injuries involve soft tissue- tendons, muscles and ligaments. Fractures, herniated discs and degenerative disc disease in more seasoned athletes are typical. These injuries can present in many different ways. Some may have pain with movement, others may have relief with movement in certain directions. The pain might feel better with standing or worse with sitting. It is important to accurately identify what structure might be causing pain and to treat it accordingly
Grappling requires a balance between very flexible, but strong hips. In the guard your hips are in flexion, abduction and relative external rotation. As your opponent is passing the guard, they may force your knee across your chest into your opposite shoulder (ex. right knee, left shoulder). This compresses the hip labrum, a soft, pliable tissue like rubber. If the labrum is torn it can cause a sharp pinching pain when you are caught in this position.
Ankle sprains occur when the foot is rolled under the body, tearing the ligament that connects the ankle to the foot. Lunging and squatting may cause this area to “pinch”. Ankle sprains typically cause the feeling of “giving way” when working your stand up game, or occasional misplacing of the foot because your brains processing of where your body is in space is disrupted.
Pain along the outside of the elbow, right on top of the radial head where the muscle mass attaches into, is called lateral epicondylagia (formerly known as epicondylitis). With tendon damage, the inflammatory phase lasts about a week and thereafter the tissue begins to heal (now no longer an “-itis”). In some injuries the tissue being laid down to replace the torn tendon is not as strong. This can lead to fraying of the tendon and fatty deposits in an attempt to stabilize the area. The fraying reduces the total amount of strength the tendon can handle. The fatty deposits alter the proper line of pull when the muscle contracts. All this being said, when you go to grab your opponents gi, wrist or leg to control it, pain hits and suddenly you cant squeeze as hard.
If you want the extended version with tips on how to prevent these injuries download The Ultimate Guide to Major MMA Injuries by Dr. Abbate.
Dr. Abbate has committed his professional career to studying all aspects of combat sports with a focus in injury prevention and rehabilitation. His broad knowledge in nutrition, strength and conditioning and psychology provides a strong foundation for athletes to refer to for support. If you are a coach or athlete in Miami, Florida and are concerned about an injury you may have sustained, Dr. Abbate is eager to provide support and care to keep you in the cage or on the mat.
Special consideration need to be taken when there is arterial bleeding (very difficult to stop, typically spurting blood) or exposure of an underlying nerve. Facial skin that has not been damage before is typically 20% as strong pre-injury at two weeks, 50% by 5 weeks and is about 80% as strong 10 weeks out. Controlling blood loss is imperative for both the fighter and the opponent. Gushing blood from a wound can cause vision to be impaired. In a fight, the cutman should have the appropriate equipment to control bleeding and swelling, especially around the eye.
Stoppage of a fight may be due to a deep laceration around the orbit or the vermillion border of the lips. Exposure of underlying nerve can result in permanent damage if not treated immediately and properly. Additionally, post-fight care should include cleaning of debris and foreign particles from the wound to prevent infection. Infection control includes use of sterile bandages, changing of bandages when necessary, maintaining a clean wound and limit training that might reopen laceration
The hand is an incredibly complex network of 29 joints, 126 ligaments, 34 tendons and their muscles, 29 bones & thick ligament-like fascia. This network allows for the manipulation of really small objects, like threading the eye of a needle, to larger objects and large movement patterns like grabbing the gi of your opponent to control them. Here is a short list of hand injuries that I often see:
Typical shoulder injuries might appear low grade at first and then rapidly deteriorate if not treated in due time. Pinching in the front of the shoulder when reaching overhead or across the chest might suggest supraspinatus (rotator cuff) impingement. The muscle is “wrung out” between two bones- the AC joint and the head of the humerus, the attachment site for the muscle. This constant pinching causes fraying of the tendon, leading to tiny tears. The body then begins to deposit fat in these tears to stabilize the area. As you might guess, fat does not do as good a job as the original tendon for transferring force from the muscle into the shoulder to produce movement (like pushing your opponent to set them up). This small tearing reduces the work capacity of the muscle and other muscles must compensate for poor movement patterns.
Neck injuries can vary from muscle aches (getting out of bed in the morning, but relief after moving around) that can be treated without any significant loss of training to severe neurological compromise requiring surgery (numbness, tingling or significant weakness of the arms or legs). Most often injuries involving the muscles can limit your ability to look around, may feel “stiff” when waking up and cause pain with certain movements, like slipping a punch. Muscular strains are often treated with hands on techniques and muscle re-education program. More serious injuries may require consultation with an orthopedic or sports medicine physician.
Combat sport athletes should be cautious of and take care of injuries in the lower back. Most back pain injuries involve soft tissue- tendons, muscles and ligaments. Fractures, herniated discs and degenerative disc disease in more seasoned athletes are typical. These injuries can present in many different ways. Some may have pain with movement, others may have relief with movement in certain directions. The pain might feel better with standing or worse with sitting. It is important to accurately identify what structure might be causing pain and to treat it accordingly
Grappling requires a balance between very flexible, but strong hips. In the guard your hips are in flexion, abduction and relative external rotation. As your opponent is passing the guard, they may force your knee across your chest into your opposite shoulder (ex. right knee, left shoulder). This compresses the hip labrum, a soft, pliable tissue like rubber. If the labrum is torn it can cause a sharp pinching pain when you are caught in this position.
Ankle sprains occur when the foot is rolled under the body, tearing the ligament that connects the ankle to the foot. Lunging and squatting may cause this area to “pinch”. Ankle sprains typically cause the feeling of “giving way” when working your stand up game, or occasional misplacing of the foot because your brains processing of where your body is in space is disrupted.
Pain along the outside of the elbow, right on top of the radial head where the muscle mass attaches into, is called lateral epicondylagia (formerly known as epicondylitis). With tendon damage, the inflammatory phase lasts about a week and thereafter the tissue begins to heal (now no longer an “-itis”). In some injuries the tissue being laid down to replace the torn tendon is not as strong. This can lead to fraying of the tendon and fatty deposits in an attempt to stabilize the area. The fraying reduces the total amount of strength the tendon can handle. The fatty deposits alter the proper line of pull when the muscle contracts. All this being said, when you go to grab your opponents gi, wrist or leg to control it, pain hits and suddenly you cant squeeze as hard.
If you want the extended version with tips on how to prevent these injuries download The Ultimate Guide to Major MMA Injuries by Dr. Abbate.
Dr. Abbate has committed his professional career to studying all aspects of combat sports with a focus in injury prevention and rehabilitation. His broad knowledge in nutrition, strength and conditioning and psychology provides a strong foundation for athletes to refer to for support. If you are a coach or athlete in Miami, Florida and are concerned about an injury you may have sustained, Dr. Abbate is eager to provide support and care to keep you in the cage or on the mat.
There has been an explosion of research regarding the assessment, treatment and effects of concussions. Concussions occur from a blow to the head and can be linear (forward/backward; think of throwing a jab or cross to the front of the face) or rotational (spinning; think of a hook or roundhouse kick to the side of the head). Linear acceleration causes bruises of the brain, disruption of blood flow to the cerebellum (responsible for balance) and nerves damage in the brainstem (area responsible for breathing, sleeping). Damage from rotational blows may stretch and tear the veins, resulting in nerve damage and bleeding out.
Special consideration need to be taken when there is arterial bleeding (very difficult to stop, typically spurting blood) or exposure of an underlying nerve. Facial skin that has not been damage before is typically 20% as strong pre-injury at two weeks, 50% by 5 weeks and is about 80% as strong 10 weeks out. Controlling blood loss is imperative for both the fighter and the opponent. Gushing blood from a wound can cause vision to be impaired. In a fight, the cutman should have the appropriate equipment to control bleeding and swelling, especially around the eye.
Stoppage of a fight may be due to a deep laceration around the orbit or the vermillion border of the lips. Exposure of underlying nerve can result in permanent damage if not treated immediately and properly. Additionally, post-fight care should include cleaning of debris and foreign particles from the wound to prevent infection. Infection control includes use of sterile bandages, changing of bandages when necessary, maintaining a clean wound and limit training that might reopen laceration
The hand is an incredibly complex network of 29 joints, 126 ligaments, 34 tendons and their muscles, 29 bones & thick ligament-like fascia. This network allows for the manipulation of really small objects, like threading the eye of a needle, to larger objects and large movement patterns like grabbing the gi of your opponent to control them. Here is a short list of hand injuries that I often see:
Typical shoulder injuries might appear low grade at first and then rapidly deteriorate if not treated in due time. Pinching in the front of the shoulder when reaching overhead or across the chest might suggest supraspinatus (rotator cuff) impingement. The muscle is “wrung out” between two bones- the AC joint and the head of the humerus, the attachment site for the muscle. This constant pinching causes fraying of the tendon, leading to tiny tears. The body then begins to deposit fat in these tears to stabilize the area. As you might guess, fat does not do as good a job as the original tendon for transferring force from the muscle into the shoulder to produce movement (like pushing your opponent to set them up). This small tearing reduces the work capacity of the muscle and other muscles must compensate for poor movement patterns.
Neck injuries can vary from muscle aches (getting out of bed in the morning, but relief after moving around) that can be treated without any significant loss of training to severe neurological compromise requiring surgery (numbness, tingling or significant weakness of the arms or legs). Most often injuries involving the muscles can limit your ability to look around, may feel “stiff” when waking up and cause pain with certain movements, like slipping a punch. Muscular strains are often treated with hands on techniques and muscle re-education program. More serious injuries may require consultation with an orthopedic or sports medicine physician.
Combat sport athletes should be cautious of and take care of injuries in the lower back. Most back pain injuries involve soft tissue- tendons, muscles and ligaments. Fractures, herniated discs and degenerative disc disease in more seasoned athletes are typical. These injuries can present in many different ways. Some may have pain with movement, others may have relief with movement in certain directions. The pain might feel better with standing or worse with sitting. It is important to accurately identify what structure might be causing pain and to treat it accordingly
Grappling requires a balance between very flexible, but strong hips. In the guard your hips are in flexion, abduction and relative external rotation. As your opponent is passing the guard, they may force your knee across your chest into your opposite shoulder (ex. right knee, left shoulder). This compresses the hip labrum, a soft, pliable tissue like rubber. If the labrum is torn it can cause a sharp pinching pain when you are caught in this position.
Ankle sprains occur when the foot is rolled under the body, tearing the ligament that connects the ankle to the foot. Lunging and squatting may cause this area to “pinch”. Ankle sprains typically cause the feeling of “giving way” when working your stand up game, or occasional misplacing of the foot because your brains processing of where your body is in space is disrupted.
Pain along the outside of the elbow, right on top of the radial head where the muscle mass attaches into, is called lateral epicondylagia (formerly known as epicondylitis). With tendon damage, the inflammatory phase lasts about a week and thereafter the tissue begins to heal (now no longer an “-itis”). In some injuries the tissue being laid down to replace the torn tendon is not as strong. This can lead to fraying of the tendon and fatty deposits in an attempt to stabilize the area. The fraying reduces the total amount of strength the tendon can handle. The fatty deposits alter the proper line of pull when the muscle contracts. All this being said, when you go to grab your opponents gi, wrist or leg to control it, pain hits and suddenly you cant squeeze as hard.
If you want the extended version with tips on how to prevent these injuries download The Ultimate Guide to Major MMA Injuries by Dr. Abbate.
Dr. Abbate has committed his professional career to studying all aspects of combat sports with a focus in injury prevention and rehabilitation. His broad knowledge in nutrition, strength and conditioning and psychology provides a strong foundation for athletes to refer to for support. If you are a coach or athlete in Miami, Florida and are concerned about an injury you may have sustained, Dr. Abbate is eager to provide support and care to keep you in the cage or on the mat.
It is especially important for combat sport athletes to take proper care of their eyes. It is recommended that they undergo yearly dilatation to detect subtle changes that may result in permanent, lifelong complications if not addressed in a timely manner. Blows to the head can cause early onset glaucoma (due to increased pressure on the optic nerve); cataracts (clouding of vision over the lens blocking light entry); corneal abrasion (contact with foreign object, possible infection); and retinal detachment, holes or tears (loss of peripheral vision, onset of floaters).
There has been an explosion of research regarding the assessment, treatment and effects of concussions. Concussions occur from a blow to the head and can be linear (forward/backward; think of throwing a jab or cross to the front of the face) or rotational (spinning; think of a hook or roundhouse kick to the side of the head). Linear acceleration causes bruises of the brain, disruption of blood flow to the cerebellum (responsible for balance) and nerves damage in the brainstem (area responsible for breathing, sleeping). Damage from rotational blows may stretch and tear the veins, resulting in nerve damage and bleeding out.
Special consideration need to be taken when there is arterial bleeding (very difficult to stop, typically spurting blood) or exposure of an underlying nerve. Facial skin that has not been damage before is typically 20% as strong pre-injury at two weeks, 50% by 5 weeks and is about 80% as strong 10 weeks out. Controlling blood loss is imperative for both the fighter and the opponent. Gushing blood from a wound can cause vision to be impaired. In a fight, the cutman should have the appropriate equipment to control bleeding and swelling, especially around the eye.
Stoppage of a fight may be due to a deep laceration around the orbit or the vermillion border of the lips. Exposure of underlying nerve can result in permanent damage if not treated immediately and properly. Additionally, post-fight care should include cleaning of debris and foreign particles from the wound to prevent infection. Infection control includes use of sterile bandages, changing of bandages when necessary, maintaining a clean wound and limit training that might reopen laceration
The hand is an incredibly complex network of 29 joints, 126 ligaments, 34 tendons and their muscles, 29 bones & thick ligament-like fascia. This network allows for the manipulation of really small objects, like threading the eye of a needle, to larger objects and large movement patterns like grabbing the gi of your opponent to control them. Here is a short list of hand injuries that I often see:
Typical shoulder injuries might appear low grade at first and then rapidly deteriorate if not treated in due time. Pinching in the front of the shoulder when reaching overhead or across the chest might suggest supraspinatus (rotator cuff) impingement. The muscle is “wrung out” between two bones- the AC joint and the head of the humerus, the attachment site for the muscle. This constant pinching causes fraying of the tendon, leading to tiny tears. The body then begins to deposit fat in these tears to stabilize the area. As you might guess, fat does not do as good a job as the original tendon for transferring force from the muscle into the shoulder to produce movement (like pushing your opponent to set them up). This small tearing reduces the work capacity of the muscle and other muscles must compensate for poor movement patterns.
Neck injuries can vary from muscle aches (getting out of bed in the morning, but relief after moving around) that can be treated without any significant loss of training to severe neurological compromise requiring surgery (numbness, tingling or significant weakness of the arms or legs). Most often injuries involving the muscles can limit your ability to look around, may feel “stiff” when waking up and cause pain with certain movements, like slipping a punch. Muscular strains are often treated with hands on techniques and muscle re-education program. More serious injuries may require consultation with an orthopedic or sports medicine physician.
Combat sport athletes should be cautious of and take care of injuries in the lower back. Most back pain injuries involve soft tissue- tendons, muscles and ligaments. Fractures, herniated discs and degenerative disc disease in more seasoned athletes are typical. These injuries can present in many different ways. Some may have pain with movement, others may have relief with movement in certain directions. The pain might feel better with standing or worse with sitting. It is important to accurately identify what structure might be causing pain and to treat it accordingly
Grappling requires a balance between very flexible, but strong hips. In the guard your hips are in flexion, abduction and relative external rotation. As your opponent is passing the guard, they may force your knee across your chest into your opposite shoulder (ex. right knee, left shoulder). This compresses the hip labrum, a soft, pliable tissue like rubber. If the labrum is torn it can cause a sharp pinching pain when you are caught in this position.
Ankle sprains occur when the foot is rolled under the body, tearing the ligament that connects the ankle to the foot. Lunging and squatting may cause this area to “pinch”. Ankle sprains typically cause the feeling of “giving way” when working your stand up game, or occasional misplacing of the foot because your brains processing of where your body is in space is disrupted.
Pain along the outside of the elbow, right on top of the radial head where the muscle mass attaches into, is called lateral epicondylagia (formerly known as epicondylitis). With tendon damage, the inflammatory phase lasts about a week and thereafter the tissue begins to heal (now no longer an “-itis”). In some injuries the tissue being laid down to replace the torn tendon is not as strong. This can lead to fraying of the tendon and fatty deposits in an attempt to stabilize the area. The fraying reduces the total amount of strength the tendon can handle. The fatty deposits alter the proper line of pull when the muscle contracts. All this being said, when you go to grab your opponents gi, wrist or leg to control it, pain hits and suddenly you cant squeeze as hard.
If you want the extended version with tips on how to prevent these injuries download The Ultimate Guide to Major MMA Injuries by Dr. Abbate.
Dr. Abbate has committed his professional career to studying all aspects of combat sports with a focus in injury prevention and rehabilitation. His broad knowledge in nutrition, strength and conditioning and psychology provides a strong foundation for athletes to refer to for support. If you are a coach or athlete in Miami, Florida and are concerned about an injury you may have sustained, Dr. Abbate is eager to provide support and care to keep you in the cage or on the mat.

Are you an MMA fighter or coach who’s looking to learn more about MMA’s most common injuries? With A Quick Reference Guide to MMA Injuries you will be able to identify and recognize several types.
Mixed martial arts and their component practices include boxing, wrestling, Brazilian Jiu-Jitsu and Muay Thai. Athletes are driven by the need to participate in tactical and technical training to develop a strong base and improve their skills.
Most injuries suffered by MMA athletes typically occur during training. Half of the injuries reported occur in the face, hands, nose and eyes. The most frequent lesions are skin lacerations, followed by fractures and concussions.
In this Reference Guide I will speak to the most common injuries that I see in training and competition.
It is especially important for combat sport athletes to take proper care of their eyes. It is recommended that they undergo yearly dilatation to detect subtle changes that may result in permanent, lifelong complications if not addressed in a timely manner. Blows to the head can cause early onset glaucoma (due to increased pressure on the optic nerve); cataracts (clouding of vision over the lens blocking light entry); corneal abrasion (contact with foreign object, possible infection); and retinal detachment, holes or tears (loss of peripheral vision, onset of floaters).
There has been an explosion of research regarding the assessment, treatment and effects of concussions. Concussions occur from a blow to the head and can be linear (forward/backward; think of throwing a jab or cross to the front of the face) or rotational (spinning; think of a hook or roundhouse kick to the side of the head). Linear acceleration causes bruises of the brain, disruption of blood flow to the cerebellum (responsible for balance) and nerves damage in the brainstem (area responsible for breathing, sleeping). Damage from rotational blows may stretch and tear the veins, resulting in nerve damage and bleeding out.
Special consideration need to be taken when there is arterial bleeding (very difficult to stop, typically spurting blood) or exposure of an underlying nerve. Facial skin that has not been damage before is typically 20% as strong pre-injury at two weeks, 50% by 5 weeks and is about 80% as strong 10 weeks out. Controlling blood loss is imperative for both the fighter and the opponent. Gushing blood from a wound can cause vision to be impaired. In a fight, the cutman should have the appropriate equipment to control bleeding and swelling, especially around the eye.
Stoppage of a fight may be due to a deep laceration around the orbit or the vermillion border of the lips. Exposure of underlying nerve can result in permanent damage if not treated immediately and properly. Additionally, post-fight care should include cleaning of debris and foreign particles from the wound to prevent infection. Infection control includes use of sterile bandages, changing of bandages when necessary, maintaining a clean wound and limit training that might reopen laceration
The hand is an incredibly complex network of 29 joints, 126 ligaments, 34 tendons and their muscles, 29 bones & thick ligament-like fascia. This network allows for the manipulation of really small objects, like threading the eye of a needle, to larger objects and large movement patterns like grabbing the gi of your opponent to control them. Here is a short list of hand injuries that I often see:
Typical shoulder injuries might appear low grade at first and then rapidly deteriorate if not treated in due time. Pinching in the front of the shoulder when reaching overhead or across the chest might suggest supraspinatus (rotator cuff) impingement. The muscle is “wrung out” between two bones- the AC joint and the head of the humerus, the attachment site for the muscle. This constant pinching causes fraying of the tendon, leading to tiny tears. The body then begins to deposit fat in these tears to stabilize the area. As you might guess, fat does not do as good a job as the original tendon for transferring force from the muscle into the shoulder to produce movement (like pushing your opponent to set them up). This small tearing reduces the work capacity of the muscle and other muscles must compensate for poor movement patterns.
Neck injuries can vary from muscle aches (getting out of bed in the morning, but relief after moving around) that can be treated without any significant loss of training to severe neurological compromise requiring surgery (numbness, tingling or significant weakness of the arms or legs). Most often injuries involving the muscles can limit your ability to look around, may feel “stiff” when waking up and cause pain with certain movements, like slipping a punch. Muscular strains are often treated with hands on techniques and muscle re-education program. More serious injuries may require consultation with an orthopedic or sports medicine physician.
Combat sport athletes should be cautious of and take care of injuries in the lower back. Most back pain injuries involve soft tissue- tendons, muscles and ligaments. Fractures, herniated discs and degenerative disc disease in more seasoned athletes are typical. These injuries can present in many different ways. Some may have pain with movement, others may have relief with movement in certain directions. The pain might feel better with standing or worse with sitting. It is important to accurately identify what structure might be causing pain and to treat it accordingly
Grappling requires a balance between very flexible, but strong hips. In the guard your hips are in flexion, abduction and relative external rotation. As your opponent is passing the guard, they may force your knee across your chest into your opposite shoulder (ex. right knee, left shoulder). This compresses the hip labrum, a soft, pliable tissue like rubber. If the labrum is torn it can cause a sharp pinching pain when you are caught in this position.
Ankle sprains occur when the foot is rolled under the body, tearing the ligament that connects the ankle to the foot. Lunging and squatting may cause this area to “pinch”. Ankle sprains typically cause the feeling of “giving way” when working your stand up game, or occasional misplacing of the foot because your brains processing of where your body is in space is disrupted.
Pain along the outside of the elbow, right on top of the radial head where the muscle mass attaches into, is called lateral epicondylagia (formerly known as epicondylitis). With tendon damage, the inflammatory phase lasts about a week and thereafter the tissue begins to heal (now no longer an “-itis”). In some injuries the tissue being laid down to replace the torn tendon is not as strong. This can lead to fraying of the tendon and fatty deposits in an attempt to stabilize the area. The fraying reduces the total amount of strength the tendon can handle. The fatty deposits alter the proper line of pull when the muscle contracts. All this being said, when you go to grab your opponents gi, wrist or leg to control it, pain hits and suddenly you cant squeeze as hard.
If you want the extended version with tips on how to prevent these injuries download The Ultimate Guide to Major MMA Injuries by Dr. Abbate.
Dr. Abbate has committed his professional career to studying all aspects of combat sports with a focus in injury prevention and rehabilitation. His broad knowledge in nutrition, strength and conditioning and psychology provides a strong foundation for athletes to refer to for support. If you are a coach or athlete in Miami, Florida and are concerned about an injury you may have sustained, Dr. Abbate is eager to provide support and care to keep you in the cage or on the mat.

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
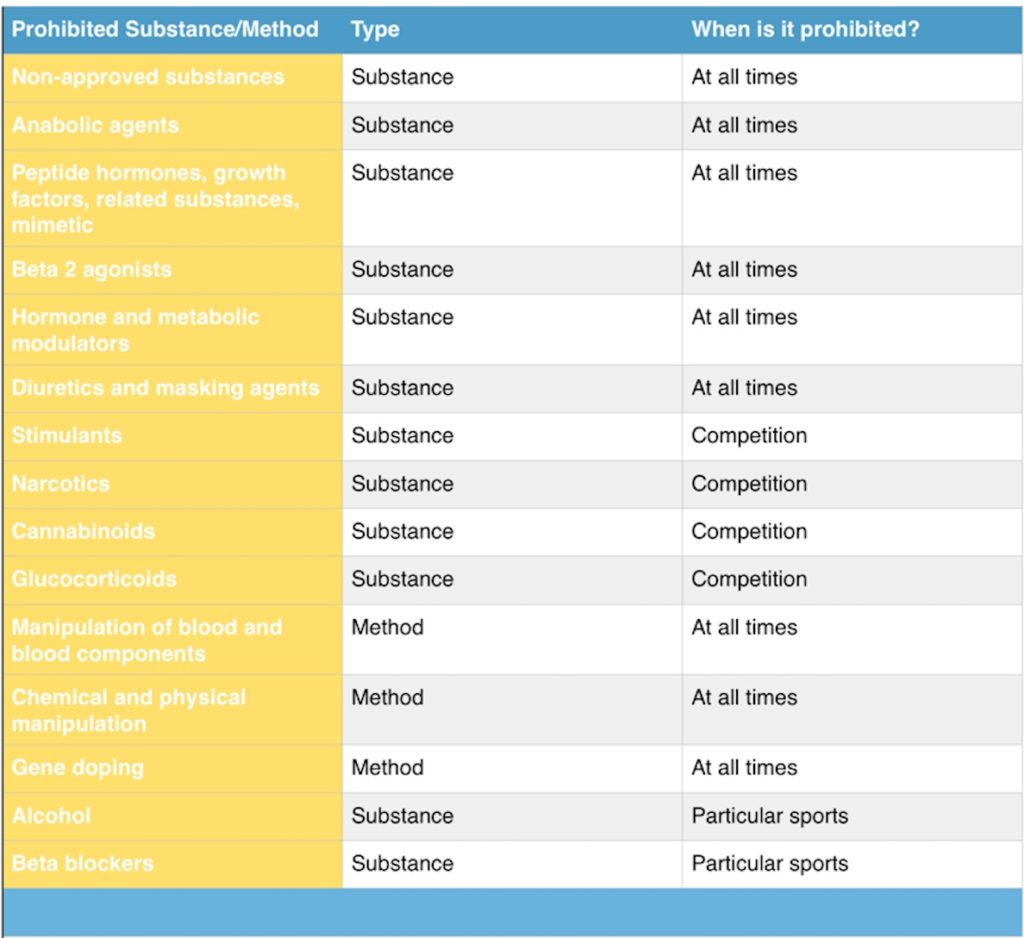
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
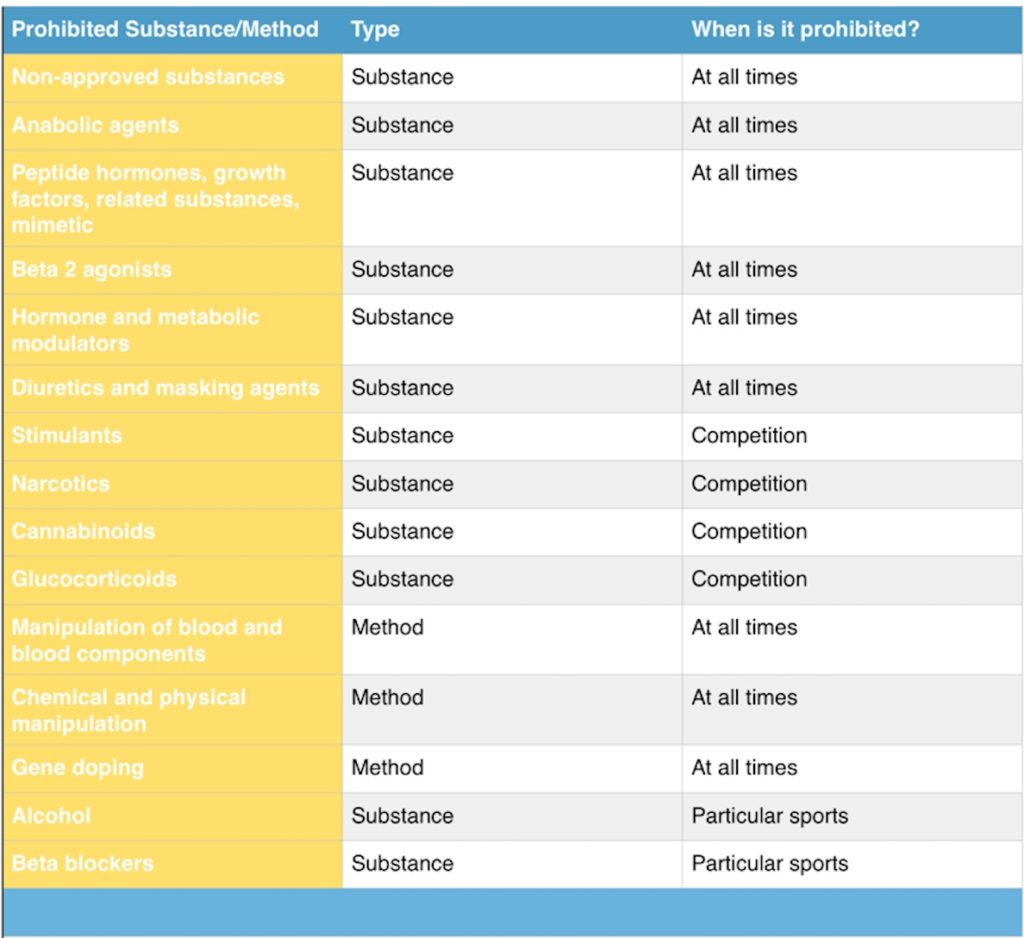
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
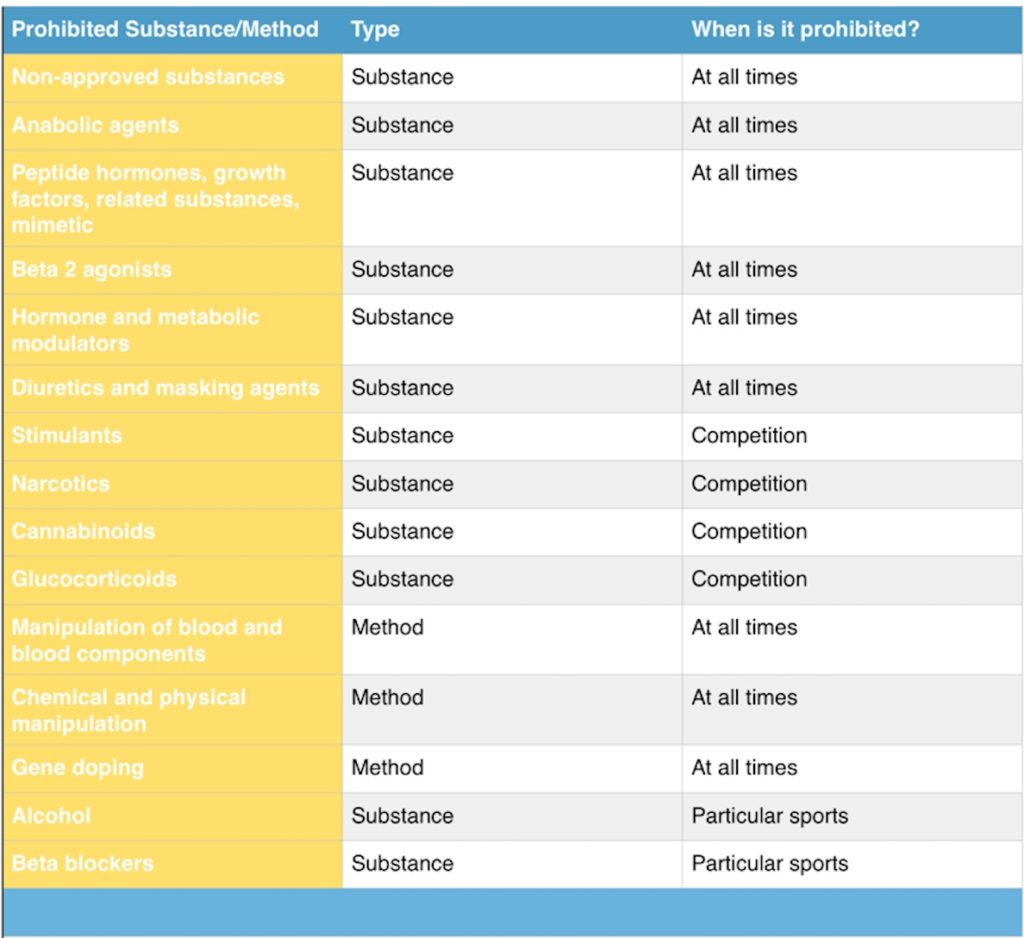
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
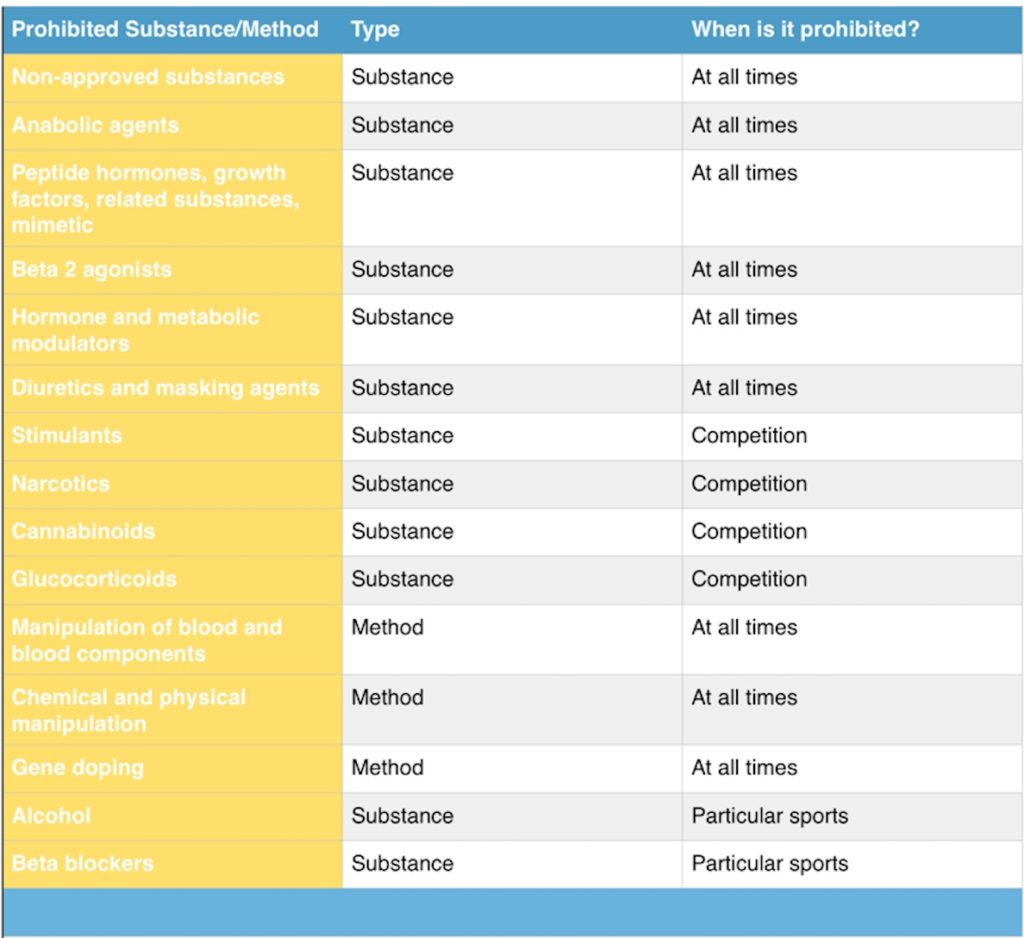
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
The United States Anti-Doping Agency (USADA) and the World Anti-Doping Agency (WADA) publish a list of banned substances or procedures yearly. The National Collegiate Athletic Association and most professional leagues produce similar categories of banned substances.
Supplements are prohibited if they meet 2 of the 3 criteria:
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
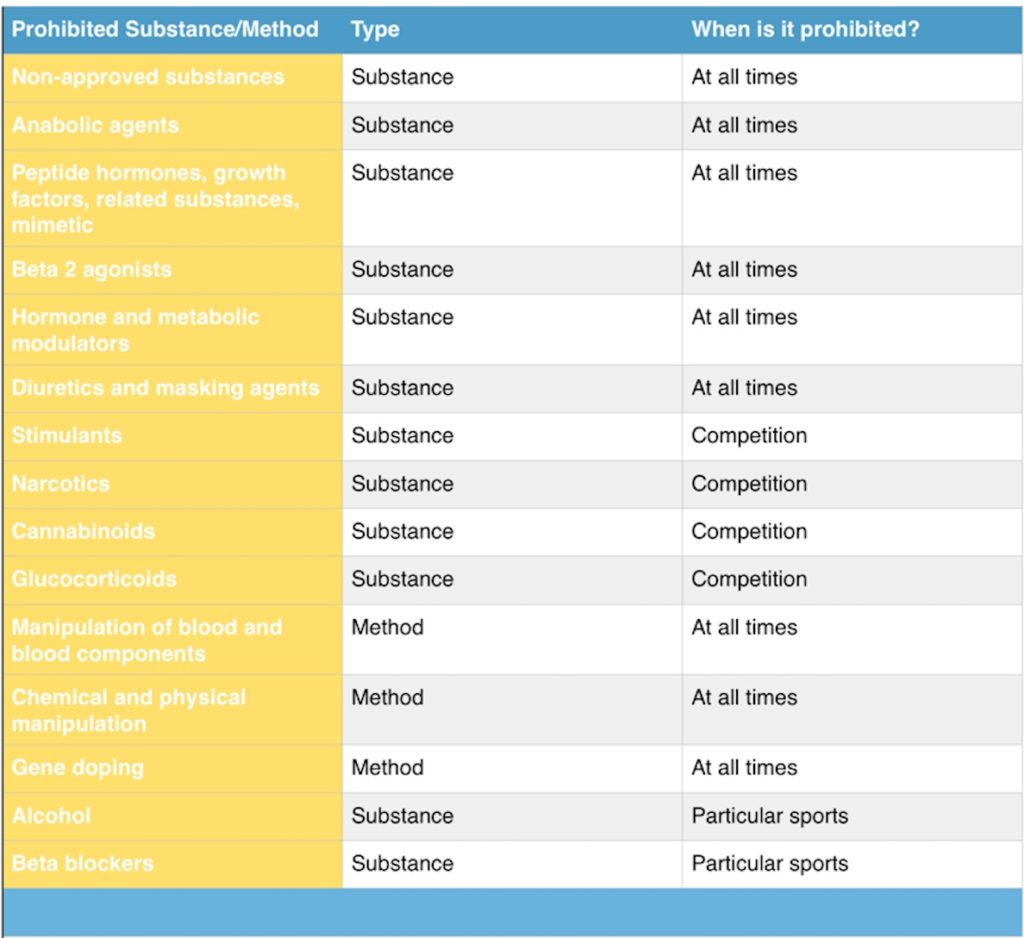
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
In 2008 Jessica Hardy, an Olympic hopeful, was banned from the Olympics and served a 1 year suspension after taking supplements for improving muscle strength and muscle mass. Jessica had taken Advocare Arginine Extreme (sounds kind of extreme), but only after researching the product, consulting with the team nutritionist, the team psychologist and even contacting the company regarding its safe and purity. Yet, she was banned from the Olympic Games… How did that happen?
The United States Anti-Doping Agency (USADA) and the World Anti-Doping Agency (WADA) publish a list of banned substances or procedures yearly. The National Collegiate Athletic Association and most professional leagues produce similar categories of banned substances.
Supplements are prohibited if they meet 2 of the 3 criteria:
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
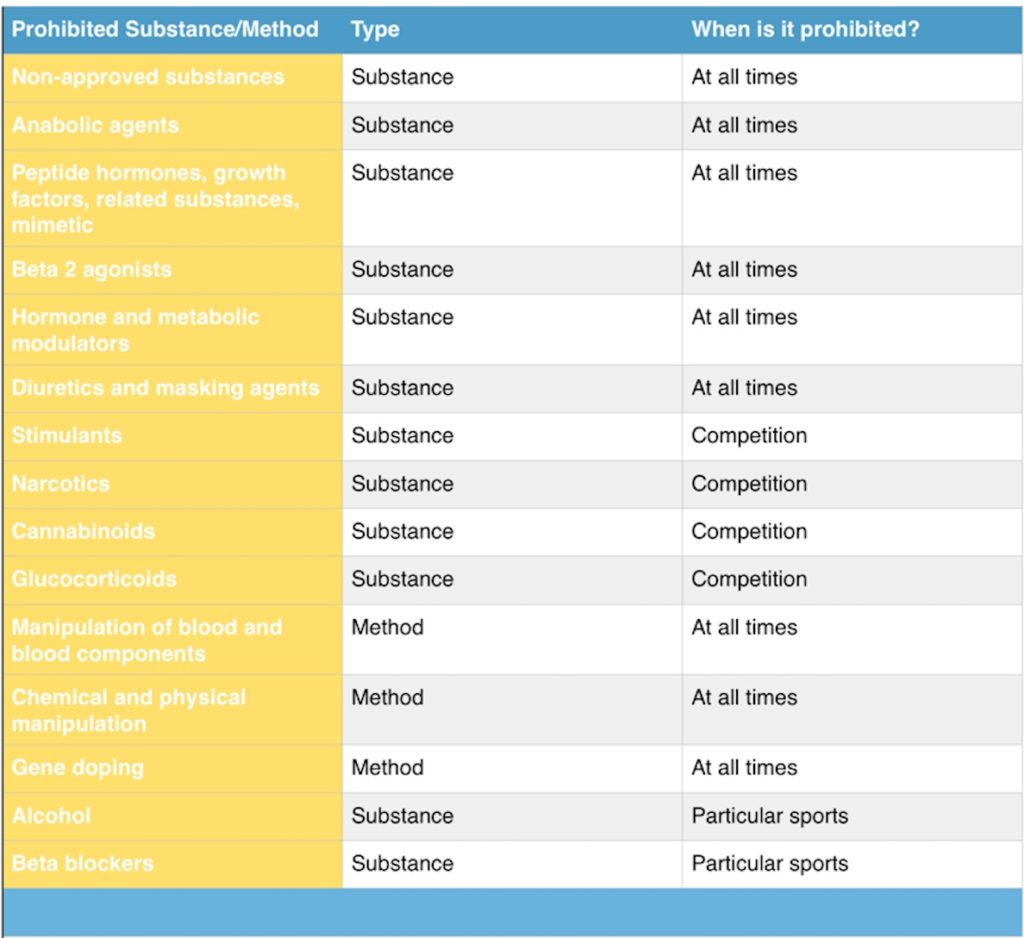
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
As an athlete are you 100% certain that the supplement you’re taking is not contaminated?
With the Winter Olympics just starting, and a recent scandal with doping on Russian Olympic Team, there are many people wondering how the Olympic committee tests for substances and what substances or methods are prohibited.
In this article we will discuss what substances are banned, and how you, as an athlete, can be affected by organizations making the determination if the supplements you are taking are allowed in your sport.
In 2008 Jessica Hardy, an Olympic hopeful, was banned from the Olympics and served a 1 year suspension after taking supplements for improving muscle strength and muscle mass. Jessica had taken Advocare Arginine Extreme (sounds kind of extreme), but only after researching the product, consulting with the team nutritionist, the team psychologist and even contacting the company regarding its safe and purity. Yet, she was banned from the Olympic Games… How did that happen?
The United States Anti-Doping Agency (USADA) and the World Anti-Doping Agency (WADA) publish a list of banned substances or procedures yearly. The National Collegiate Athletic Association and most professional leagues produce similar categories of banned substances.
Supplements are prohibited if they meet 2 of the 3 criteria:
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
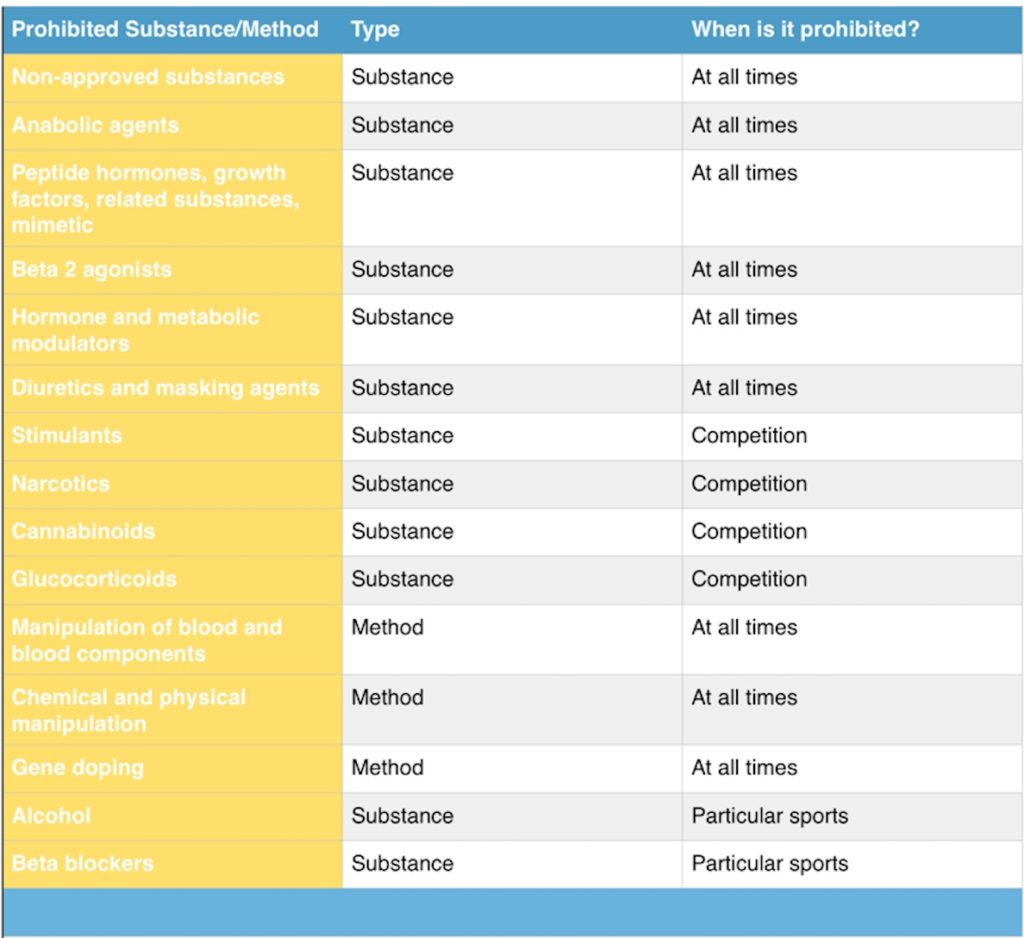
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.
As an athlete are you 100% certain that the supplement you’re taking is not contaminated?
With the Winter Olympics just starting, and a recent scandal with doping on Russian Olympic Team, there are many people wondering how the Olympic committee tests for substances and what substances or methods are prohibited.
In this article we will discuss what substances are banned, and how you, as an athlete, can be affected by organizations making the determination if the supplements you are taking are allowed in your sport.
In 2008 Jessica Hardy, an Olympic hopeful, was banned from the Olympics and served a 1 year suspension after taking supplements for improving muscle strength and muscle mass. Jessica had taken Advocare Arginine Extreme (sounds kind of extreme), but only after researching the product, consulting with the team nutritionist, the team psychologist and even contacting the company regarding its safe and purity. Yet, she was banned from the Olympic Games… How did that happen?
The United States Anti-Doping Agency (USADA) and the World Anti-Doping Agency (WADA) publish a list of banned substances or procedures yearly. The National Collegiate Athletic Association and most professional leagues produce similar categories of banned substances.
Supplements are prohibited if they meet 2 of the 3 criteria:
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
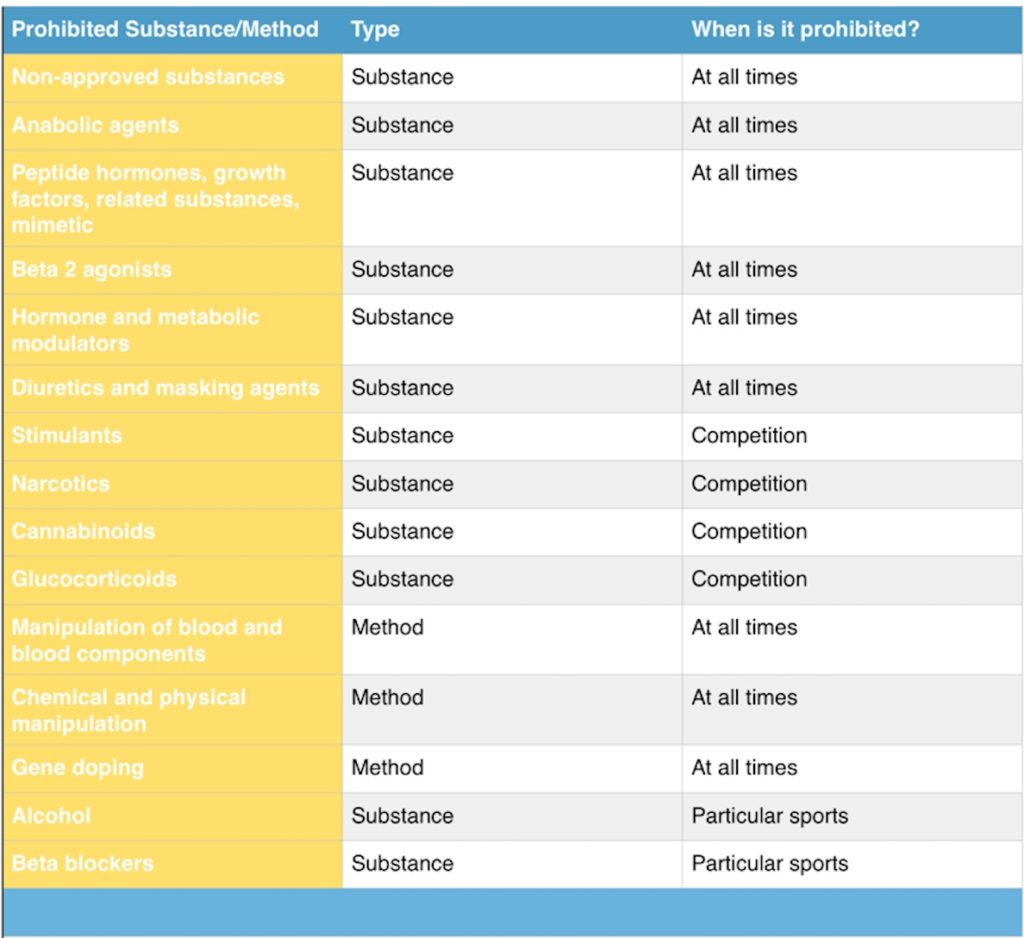
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.

Are you one of the 94% of athletes taking supplements?
Do you take supplements because you want to…
As an athlete are you 100% certain that the supplement you’re taking is not contaminated?
With the Winter Olympics just starting, and a recent scandal with doping on Russian Olympic Team, there are many people wondering how the Olympic committee tests for substances and what substances or methods are prohibited.
In this article we will discuss what substances are banned, and how you, as an athlete, can be affected by organizations making the determination if the supplements you are taking are allowed in your sport.
In 2008 Jessica Hardy, an Olympic hopeful, was banned from the Olympics and served a 1 year suspension after taking supplements for improving muscle strength and muscle mass. Jessica had taken Advocare Arginine Extreme (sounds kind of extreme), but only after researching the product, consulting with the team nutritionist, the team psychologist and even contacting the company regarding its safe and purity. Yet, she was banned from the Olympic Games… How did that happen?
The United States Anti-Doping Agency (USADA) and the World Anti-Doping Agency (WADA) publish a list of banned substances or procedures yearly. The National Collegiate Athletic Association and most professional leagues produce similar categories of banned substances.
Supplements are prohibited if they meet 2 of the 3 criteria:
The WADA code places the burden of proof on the athlete to perform due diligence for any supplement or substance that enters their body. While the majority of doping cases are accidental, some 8% of doping are due to tainted supplements.
A supplement is defined as a product intended to augment the diet that bears or contains 1 or more of the following:
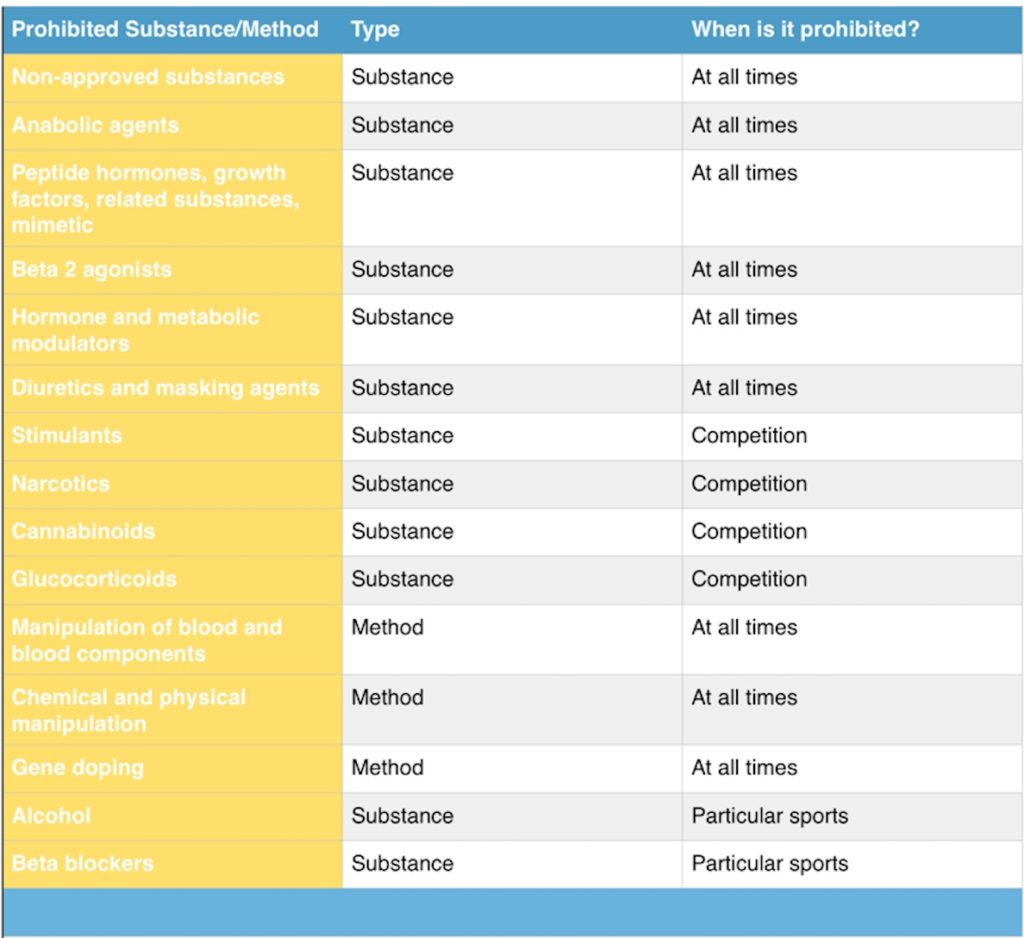
Not sure what a beta 2 agonist or some of the other substances/methods mentioned above? Keep an eye out for my upcoming articles on sports supplementation.
The Dietary Supplement Health and Education Act (DSHEA) of 1994 regulates dietary supplements as a food, not as a pharmaceutical drug. Therefore, they do not require FDA approval before producing or selling dietary supplements. They also do not require studies to demonstrate if the supplement actually works.
So the DSHEA is intended to provide access to safe dietary supplements, improving the health of Americans, empowering consumers to make choices about preventative health and stimulating the growth in the dietary supplements industry.
Supplements cannot claim to diagnose, treat, cure or prevent any diseases.
Yet:
Athletes are often uninformed or misinformed regarding supplement use, the side-effects of supplements and the quality of supplements.
Even on the medical side, physicians are ill informed.
Between 2004 and 2013 an estimated 23,000 visits to the ER and 2136 hospitalizations were due to adverse effects of supplements. They were most often due to weight loss and energy supplements.
Hepatotoxicity, or liver injury, was most often the cause of hospitalization.
Doping can result from ingestion of a banned substance, either intentionally or unintentionally, passively (second hand smoke), tainted food, or just being a superhuman and having abnormally high levels.
Contamination also occurs on the manufacturers end. This can be due to poor manufacturing practices or manufacturers purposely spiking supplements.
Tainted substances also occur in non-performance enhancing supplements. Sexual enhancement and weight loss account for 46% and 39% of contaminated substances according to the FDA Tainted Supplements List.
Third party companies assess supplements for quality, purity, potency and composition. A “seal of approval” is issued and can be displayed on the product label. This process is voluntary.
Thats great, but two issues come up: small companies, may not be able to pay fees for the seal; larger companies, already in the market, might not see any value.
Check for the following seals to determine whether or not the supplement has passed the testing process:
A few more things…

What they do:
BSCG’s Certified Drug Free® supplement certification programs fill a significant gap in dietary supplement quality control and aim to help average consumers and elite athletes alike differentiate safe products from those products that present unnecessary risks with pragmatic supplement information. BSCG is pleased never to have certified a product that went on to cause a positive drug test. We use the most up-to-date science to provide manufacturers and consumers with the best protection available against these risks.

What they do:
ConsumerLab.com has perhaps the highest testing standards of any third party group certifying the quality of dietary supplements. ConsumerLab.com is also the only third-party verification group that freely publishes its testing methods and quality criteria/standards. These can be found at www.consumerlab.com/methods_index.asp.
Products are tested, whenever possible, for each of the following:
-Identity: Does the product meet recognized standards of identity and does the product meet the level of quality claimed on the label?
-Strength (quantity): Does the product contain the amount of ingredient claimed on the label?
-Purity: Is the product free of specified contaminants?
-Disintegration: Does the product break apart properly so that it may be used by the body? [See ConsumerLab.com Home Test for Disintegration for how to test your supplements]

Informed-Choice tests products/ingredients for a range of substances that appear on the WADA Prohibited List, as well as lists from organizations such as the AFL, NRL, NFL, NCAA, and MLB. Substances may be included in the testing specification for a number of reasons, including:
•They are/were sold as a supplement (e.g.. androstenedione, DHEA)
•They have been reported as a contaminant in a supplement (e.g.. 19-nor-androstenedione, stanozolol)
•They have been the subject of widespread publicity linking them with adverse analytical findings and/or supplements (e.g.. THG, nandrolone)
•They are widely available as a recreational drug and are potentially at a higher risk of being a contaminant (e.g.. cocaine, ecstasy)
•They have been reported as an adverse analytical finding (e.g.. clenbuterol, strychnine, salbutamol, terbutaline)
•They are chemically closely related to any of the substances above (e.g.. isomers, parent drugs, etc.)

What they do:
Accredited by the American National Standards Institute (ANSI), NSF has developed over 70 currently active voluntary American National Standards under the scope of public health, safety, environment and sustainability assessment. NSF/ANSI standards are developed through a public process that ensures balanced input from industry representatives, public health/regulatory officials and users/consumer representatives.

What they do:
Safeguarding supply chains and boosting consumer confidence in dietary supplement products. They’re just two ways that USP Dietary Supplement Verification Services benefit those who work with and use dietary ingredients and finished supplement products each day.
Offered to manufacturers and brands worldwide, USP Dietary Supplement Verification Services include GMP facility auditing, product quality control and manufacturing product documentation review, and product testing. Participation is voluntary and products that meet USP’s stringent requirements are awarded the distinctive USP Verified Mark, making it easy for suppliers and consumers to spot quality they can trust.

Have you ever been injured and not sure what the first step should be?
How do you know if you should see a medical doctor, physical therapist, massage therapist or a chiropractor? Do you ask your coach for advice?
Or maybe you just take off time from your sport?
Whatever you choose to do, it is important that you make an informed decision. There are many phenomenal clinicians out there, as well as a handful of fakes.
But how do you spot the difference?
Here are three things you should ALWAYS consider when seeking advice
1. What are the persons credentials?
With the internet of everything, it is easy to have access to information through memes, blogs, Instagram or Facebook posts. There are tons of certifications, self-proclaimed gurus and “Masters of yahyahyah”.
Here are two ways you can differentiate between a gym-bruh and a professional.
A certification is the recognition that the individual has completed some type of examination by a particular company or organization. Sometimes these certifications are legit, others, not at all. Most certifications have to clear a minimum standard for education or complete certain requirements. These include personal training certifications, CPR training, or a particular type of technique or treatment (kinesiotaping).
Licensure is the recognition that the individual has completed some type of formal training that meets minimum standards set forth by the state in which they received the license. The great state of Florida, for example, has certain criteria that need to be met for physicians, physical therapists and chiropractors to practice. These academic programs are vetted by a rigorous process that includes committees or professional organizations that have a long history within that field, provide research in that area and are constantly updating their curriculum to reflect best practices. The clinician will have to undergo years of formal classes and an internship where they are guided by other clinicians to ensure a level of understanding that is needed to practice.
It is best to seek advice from someone who has formal training, where they were tested by professionals in their field.
2. What are they telling you?
You spoke to them for 0.3 seconds and they are “diagnosing” you.
Calmly thank them for their expertise and back away… slowly. They might bite!
No legitimate professional will offer any diagnosis or treatment options without first having a solid “getting to know you” conversation. It is important that the questions they ask are relevant and important to you, the condition you (may) have and your concerns at that time, then and there.
A good clinician will take the time to understand you- what sports you play, performances you’ve done, competitive events, goals and fears. Your experience with injuries, what has worked and what hasn’t worked in the past.
At this stage, they should be doing a lot of listening. Not so much talking.
3. Does the information and suggestions they offer make sense.
Are you telling them how you have shoulder pain when pushing yourself off the floor and they keep telling you about x, y, or z treatment, but there seems to be no connection between the two?
Unless they can guide you through a common-sense treatment process, I would be cautious. Ask them a few questions, give them an opportunity to explain further, maybe the plan of care needs to be cleared up from being a little fuzzy.
Ask them what exactly is going on and how exactly they plan to help you.
Your body, your decision.
At the end of the day, it is your body and you have the ultimate decision on what you want to do or don’t want to do. Consider what you are learning from what the clinician is telling you- it should make sense to you at that time and place with the injury you have.
As a clinician treating elite performing artists, gymnasts and combat sports athletes for the past 8 years, I am ALWAYS eager to answer their questions and guide them through the decision making, injury pathology and recovery process.
Because I truly care.

I am often asked about diet, cutting weight and healthy ways to go about it. While I am not a nutritionist or dietitian and cannot offer you specific dietary advice, I have had a lot of experience making weight for wrestling and BJJ competitions. The advice I offer below are guidelines for healthy methods. It is not a comprehensive meal plan or specific directions on what you should do.
Consultation with a professional is ALWAYS the best option. If you know of anyone, feel free to send me their website or contact info, I’m always looking for other health care professionals to work with.
That being said, be careful of “gurus” offering advice that have no background in health or fitness, and only offer suggestions based on their experience only.
So lets get to the meat of it!
Combat sports, especially weight-class based sports including MMA, boxing, BJJ, kickboxing, Muay Thai and wrestling have various training & competitive seasons.
Some seasons can last months, like in wrestling, where a competitor has a long time to plan their weight training, technique and nutrition in neat cycles. Or it can be a few short weeks, like for amateur MMA athletes that are called a week before due to a card drop out.
All of these scenarios have their own unique set of challenges. Properly supplying your body with high quality energy during workouts and recovering from training are paramount to success for each fight as well as over the course of a fighters career.
Don’t get burnt out! You might not care now, but your lifestyle at this very moment can prevent a hell of a lot of trouble when you’re still competing at 50, 60 or even 70 years old! The benefits of being a lifelong athlete are too numerous to be listed in this blog (which is why I will be writing on up on cultivating athleticism in a few weeks)!
Below I review 4 common weight making issues and solutions to address them.
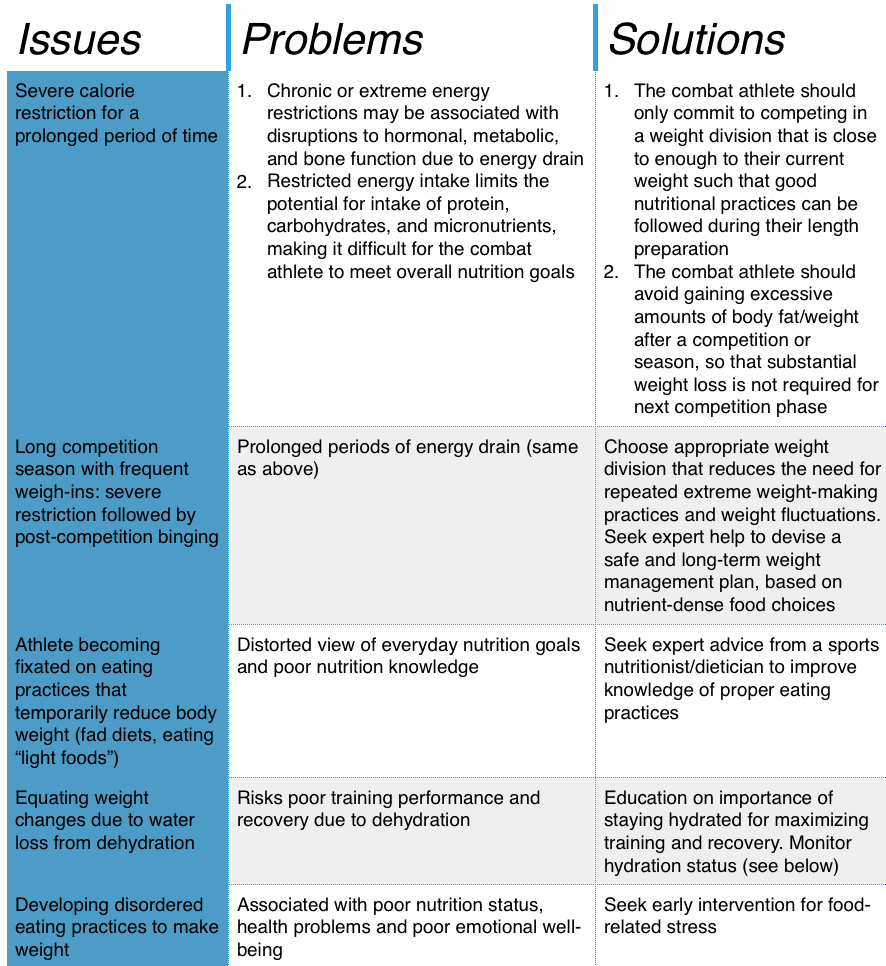
Having a nutritionist or dietician who is familiar with your sport and understands the demands of multiple training sessions will keep your body healthy & limit the risk of injury. Its important that you feel like you have the energy to practice without feeling mentally drained or lose the desire to compete.
Calorie restriction, if done improperly, can lead to moodiness, irritability, overtraining & early burnout. If severe enough, overtraining can last months and ruin your career.
Here are a few tips for eating for safe, long term loss of body weight/fat:
Traveling can also be an issue with maintaining clean eating habits. Plan ahead when traveling by planning meals or knowing what restaurants serve before going to your destination. If possible, consider packing home-foods that might not be available at your destination.
Enjoy this article?
Want to see more of it?
Think a training partner can benefit from it?
Feel free to share it.
Cultivate athleticism,
Cory Abbate, DPT, COMT, BS Ex Sci, EMR











